The Effectiveness of Standard Cognitive Analytic Therapy (CAT) with people with mild and moderate acquired brain injury (ABI): an outcome evaluation.
Rice-Varian, C., 2011. The Effectiveness of Standard Cognitive Analytic Therapy (CAT) with people with mild and moderate acquired brain injury (ABI): an outcome evaluation.. Reformulation, Summer, pp.49-54.
Abstract
Three people with mild to moderate acquired brain injury (ABI) were selected from the Community Brain Injury Service client group for a standard sixteen session Cognitive Analytic Therapy (CAT). Two of the outcome measures - HADS and C.O.R.E - showed that all clients demonstrated an improvement post therapy, whereas the third - SF–36 -showed a mixed pattern of results. Qualitative results are also presented together with comments on the work from my CAT supervisor. CAT proved to be a beneficial individual psychological intervention with these three clients.
Introduction
The theory and practice of CAT arose out of the psychotherapy outcome measures research of Anthony Ryle in the 1970’s. It is suited to being adapted to meet the specific needs of a range of client groups in the NHS. Ryle and Kerr (2002 p.1) write,
“The model arose from a continuing commitment to research into effective therapies and from a concern with delivering appropriate, time-limited, treatment in the public sector. Originally developed as a model of individual therapy, CAT now offers a general theory of psychotherapy with applicability to a wide range of conditions in many different settings.”
The CAT model and its therapy have been modified to meet the needs of client groups such as people with a diagnosis of Borderline Personality Disorder (Ryle 1997a, 1997b), mild and moderate learning disability, (Crowley, et al. 2002), people with psychosis, (Kerr 2001), in old age and early dementia, (Sutton 1997), and people with substance abuse issues (Leighton 1997). CAT has also proved beneficial with people with medical conditions such as diabetes (Fosbury et al. 1997), and asthma (Cluley et al. 2000), where non-compliance with treatment regimes can have serious life threatening consequences.
Ryle and Kerr (op. cit p. 216) acknowledge CAT’s diversity and utility and write:
“Owing to its rapid expansion in popularity CAT is now being widely used to treat many conditions very successfully without, as noted recently, having gone through the phase of undergoing strictly controlled randomized trials (Margison, 2000). This is partly due to the popularity of the model and its perceived clinical effectiveness...”
Yeates et al (2008) present two case studies, including an outcome evaluation, of clients with dysexecutive difficulties following Acquired Brain Injury (ABI). A clinical reformulation linking CAT with a neuro-psychological model was used with the clients, including a formulation linking early and current relationships. The authors concluded that CAT might be a helpful therapeutic framework for further cases but did not give details of the severity of the clients’ brain injury. One client, who was living at home, received external prompts via his mobile phone to alert him to the danger of enacting a negative procedure and thus helped him avoid arguments with his spouse. The other client lived in a residential home and the staff acted as the external prompts to support the client in switching out of a negative role state.
Quraishi (2009) summarized the types of papers that have formed the evidence base for CAT into four types: Randomised Control Studies (RCTs), Comparative Studies, Evaluations of effectiveness of CAT, and Single and Multiple Case Studies, and then Other Studies and Reviews. The current study is an evaluation of effectiveness of CAT with clients with mild and moderate ABI living in the community in their own homes and undergoing community rehabilitation.
Initially, I felt daunted by the prospect of being in the “hero innovator” role (referred to in Jellema et al. 2003) by practising CAT with a new client group. I had only recently qualified as a CAT Practitioner and community brain injury was a relatively new specialism for me at the time. The majority of my working life had been as an Occupational Therapist working in mental health. With the encouragement and support of our Neuropsychologist and my CAT Supervisor, and with the appropriate procedures in place both ethically and managerially, I went ahead with my first referral for initial assessment for CAT.
Outcome measures selection
The outcome measures selected were the Hospital Anxiety and Depression Scale (HADS) (Zigmond and Snaith 1983), The Short Form 36 health survey questionnaire (SF-36), (Anderson et al. 1996), and the Clinical Outcomes in Routine Evaluation (CORE) (CORE Partnership 2007). One of our Neuropsychologists advised us on and supported the selection of these measures.
Ethical considerations and Clinical Supervision
A proposal was written and accepted by the senior clinical staff to consider whether a standard CAT (16 sessions) would be an effective therapy for three individual clients with mild to moderate ABI. It is normal practice for our client group to have outcome measures pre-and post-treatment so this study was felt to be an example of good practice rather than a research study per se. My CAT Supervisor was in agreement with this and supported the selection of the clients. The clients were selected from the current Community ABI case loads. The criteria for selection were based on clients having two or more of the following criteria: i) showing psychological/emotional distress following their brain injury; ii) having engaged with ‘standard’ practice of Neuropsychology and Occupational Therapy interventions but needing to work on underlying issues which were negatively influencing their community rehabilitation; iii) having clear rehabilitation goals such as vocational goal/job retention issues; and/or iv) experiencing role change issues with a partner, parental role etc. as a result of their brain injury.
Other considerations for the use of CAT with people with a mild to moderate ABI
The unique trauma of having an acquired brain injury must be the often “overnight” change in the clients’ sense of self, their identity and the changes associated with their cognition, and physical impairment. Usually they have experienced a life threatening event or illness which caused their brain injury. Clients are often driven to recover and be “the person they used to be”. They quite often will make negative comparisons between how they are post-injury and how they were before it. This makes recovery from brain injury a complex, many-faceted and often chaotic time for clients, their families and their social networks. Coetzer (2008) feels that this search for identity is the central issue in brain injury rehabilitation in the community.
Clients talk about having “lost sight of themselves” or of “being unrecognizable”. This is akin to “The Hero’s Journey” referred to by Malia and Brannagan (2007).
I considered that issues of loss and acceptance and adjustment to a change in clients` sense of self could be addressed by time-limited CAT in the same way as issues of loss and grief. Writing about unresolved mourning, Ryle and Kerr (op cit., p.160) say:
“…coping requires the acceptance of the fact of loss followed by the assimilation of its meaning… The time limit of CAT, its intensity and the direct focus on loss at termination which is recorded in the ‘goodbye letter’ are all features which make it a suitable intervention for patients with problems in this area.”
I thought that the structure of CAT made it an appropriate intervention for clients recovering and coming to terms with their brain injury. The CAT was intended to facilitate clients’ acceptance and insight into their difficulties in the here and now, and to enable clients to use other aspects of their community rehabilitation more effectively. For example, it helped clients to accept using adaptive equipment and/or memory aids rather than waiting for a “magical cure”. It also helped clients to avoid putting all their energy into, say, physical therapy, or even, with some people, a denial of any problems at all.
In the therapy of people recovering from an ABI, my CAT supervisor and I considered that CAT – both therapist and structure - might support the client’s reconstruction of a new identity. It seemed to us that the “scaffolding” provided by the structure of CAT might facilitate a person’s own recovery process. This is similar to the Zone of Proximal Development (ZPD), a term coined by Vygotsky (referred to in Ryle, 1991) and defined as
“… the gap between a persons’ current performance and the level which might be attained with the assistance of a more competent other”.
CAT is a narrative therapy and as such may enable the client with an ABI to put their injury into the context of their whole life. Inferior or damaged roles may not be as long-standing in ABI as, for example, with some Older Adults or people with Learning Disabilities. and may, therefore, be more amenable to change and/or amelioration by CAT. Where an individual was coping with life in a “good enough” manner prior to their brain injury, and where their procedures have been made incomplete or ineffective owing to the ABI, an alternative procedure or exit could be developed making use of the client’s zone of proximal personality development (ZPPD). The ZPPD is a proposed extension of the ZPD (see above) and applies to the development of self processes.
Adaptations to the CAT tools and outcome measures
CAT psychotherapy tools are adaptable and flexible. One of the clients had reading difficulties as a result of their brain injury due to a form of acquired dyslexia. The Psychotherapy file, Reformulation Letter, Sequential Diagrammatic Reformulation (SDR) and Goodbye Letters (as well as the outcome measures) were all adapted for that client. King’s simplified version of the CAT Psychotherapy File (2005) was used for the client with dyslexia-like difficulties, and the outcome questionnaires were administered in A3 size in order to make it easier for the client to complete them with minimal assistance.
Once therapy was underway, Sequential Diagrammatic Reformulation (SDR) and rating scales were used in each session in the usual collaborative way.
Emergent Themes
Following a brain injury, symptoms of mental and physical fatigue are very common (Powell, 2004). Problems with fatigue are rated by clients with ABI as second in severity only to those problems caused by cognition (e.g. memory difficulties) in terms of causing them difficulties in their recovery and life following their injury. Problems with fatigue adversely affect a person’s quality of life and wellbeing. The standard educational advice from psychologists and occupational therapists - to moderate activity, take breaks and pace themselves - is overridden in some people by the need to maintain activity in a “striving procedure” as a way of keeping unmanageable feelings and unmet needs at bay, or to avoid criticism and failure. If this is the way a client has managed adverse situations or life events in their past (i.e. pre-injury), they are likely to attempt to employ the same striving procedure which they were able to use successfully prior to their ABI. This will be ineffective or only partially successful following their brain injury, as they will not have the mental or physical stamina to manage their feelings in this way. They are likely to follow a cycle of over-activity which they cannot sustain due to fatigue and headaches. At this point they may be exhausted, and low in mood, and in a state of under-activity. In CAT most clients find this under-active state may be in a “dreaded and desperately avoided” place in their SDR. They may find they are in touch with their Core Pain or unmet needs or unmanageable feelings. People who have harsh or critical self-to-self reciprocal roles may “self talk” in a critical, hostile or disparaging way. This is closely linked to increased stress and may result in low mood or depression (Gilbert 2009, 2010). They may attempt to motivate themselves out of their inactive state, wrongly labeling themselves as lazy or stupid.
The issues of control and care which some of the clients showed may have resulted in some negative interactions with allied healthcare professionals (AHPs) and medical and nursing staff. The clients in this study had elicited negative reciprocations of roles, which resulted in not getting the care they needed owing to being thought of as “difficult” or “uncooperative”. This was the case with the first CAT client who had been discharged from the care of a Consultant in London because she demanded more information regarding the evidence base for proposed tests and treatment. Another client was initially unable to accept their need for adaptive equipment such as a walking aid. Procedures of this nature may result in the client abandoning their professional carers or in their professional carers abandoning them by discharging them. This client had been previously discharged from their out-patient Physiotherapy treatment. Following CAT this client was able to have Physiotherapy and felt less self-conscious walking with a walking aid.
CAT clients in this study reported better interactions with their care network following and towards the end of their therapy. I was able to liaise with one client’s surgeon (with the permission of the client) to help him understand why he found a series of medical procedures more distressing in comparison with the surgeon’s other patients. Sharing information drawn from the client’s SDR helped to ease his distress and created more tolerance for, and understanding of, him amongst those providing his care. Another client was able to tolerate using a walking aid and engage in physiotherapy following their CAT, as one of their exits was tolerating feeling/looking vulnerable and asking others for support. Negative interactions resulted in clients not feeling listened to and their needs not being met. They were able to come to an understanding as to why they were finding adjusting to their changed sense of self following ABI so difficult to accept. In the safe space of the therapy, they were able to reflect on the fact and on the meaning of what had happened to them. The shared understanding developed in therapy enabled clients to grieve for, accept, and then start to create exits or alternative strategies for living with, their brain injury. Through the process of the therapy, clients began to become more accepting of themselves, and more able to take care of themselves and to accept help from others.
One client, who was a new parent at the time she had an ABI, was able to bond successfully with her child despite having little or no memory for the early months in her child’s first year of life.
In CAT with people recovering from a brain injury, the aim is to reunite the client with their strengths and help them to develop alternative coping strategies whilst the therapy provides the scaffolding for this process to take place. CAT may provide the scaffolding for people to develop alternative coping strategies or exits and come to terms with their brain injury and be able to accept help and care. Nehmad (2010) proposed practising “enhanced CAT” which involves explicitly eliciting from the client what their healthy roles and procedures are. The client’s SDRs include their healthy roles and procedures as well as their ineffective or unhelpful ones. CAT may facilitate their recovery and may reconnect them with their past strengths and needs as well as with their current ones.
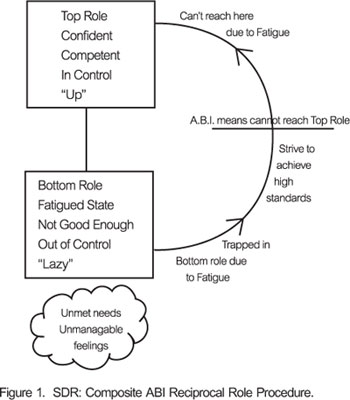
The Reciprocal Role Procedures (RRP’s) and ways of managing feelings which make recovery from mild and moderate ABI even more distressing than usual are those which involve striving and sustained action towards the desired Top Role. See Figure 1 for a composite Sequential Diagrammatic Reformulation (SDR) found with all the ABI clients. The presence of this kind of procedure may put a person at a greater risk of anxiety, depression, emotional distress and suffering, because due to brain injury fatigue the person no longer has the mental and physical stamina to enact the striving procedure. This leaves the person trapped in the Bottom Role, in the often unbearable position of being in touch with unmanageable feelings and unmet needs. In addition, they are unlikely to have a positive outcome from their brain injury rehabilitation. This evaluation found that the standard community brain injury rehabilitation intervention of advice and education regarding pacing activity to aid clients’ recovery from fatigue was not effective in these clients prior to them having CAT. Following CAT they were able to create exits from this procedure such as “feeling more and acting less” and were able to gradually increase activity and pace themselves appropriately.
The common exits from unhelpful or incomplete procedures which the ABI clients demonstrated in this study were around acceptance of how they are now in relation to how they were before their injury. This has resulted in unexpected and unrealized potential for developing in another direction both as a person but also in terms of career choice.
Results
CAT client 1: HADs, CORE and SF–36. All measures show clinically significant changes from pre - to post-therapy scores.
(See Appendix)
CAT client 2: HADs, CORE and SF–36. See Appendix. This client showed some improvement post therapy. Reasons for lower function in some areas are suggested in the discussion.
CAT client 3: HADs, CORE, and SF–36. See Appendix. Post therapy this client showed improvement. Reasons for other changes are suggested in the discussion.
CAT client 1 was able to attend for three follow-up appointments at prearranged regular intervals (one month, three month and six month post therapy) and repeated the clinical questionnaires demonstrated improvements on the post therapy score. One year post CAT they had maintained their progress, as shown by their HAD, and CORE scores which remained the same as post therapy.
Qualitative data/feedback from clients, family members and the clinical team
The clients themselves reported improvements in their level of functioning as well as wellbeing, an improved relationship with themselves and in their relationships with others close to them. (See Appendix)
Owing to the highly personal and specific nature of the individual clients’ goodbye letters, I did not feel that actual quotes from their letters would be appropriate and also might identify the clients to others reading the study. However, all clients reported finding the therapy very challenging but useful. All the clients created exits from “unhelpful” Target Problem Procedures (TPPs) such as “striving for perfectionist goals”.
Both during the working part of the therapy and post-therapy, clients reported an improvement in their acceptance of the effects of their brain injury as well as perceived improvements in concentration, memory and executive functioning. Clients were able to develop and use strategies to improve and compensate for their difficulties, often making use of previous rehabilitation advice and education. In addition, clients reported improved relationships with themselves (self to self reciprocal role procedures) and with family and clinicians (self to other reciprocal role procedures) working with them on other areas of their recovery and community brain injury rehabilitation. Unsolicited reports from family members, spouses and parents indicated improvements in all areas of functioning and relationships following the CAT. Treating clinicians also reported seeing positive changes in their clients at their out patient appointments for Neurology, Neuropsychology, and Community Occupational Therapy and Physiotherapy.
Discussion
The HAD and the CORE outcome measures demonstrate that following CAT all three clients showed improvements in their symptoms of anxiety and depression, overall wellbeing and level of functioning.
The SF–36 measures suggest that, at the time the post-therapy evaluations took place, the results may have been affected by events in the clients’ lives, along with individual differences both in the clients’ physical functioning and health issues associated with their brain injury or the cause of their brain injury.
Client 1 showed the same role physical (rp) score following therapy. This could be understood in terms of their medical condition which caused their brain injury. In other words, the client adjusted to their health condition but was still limited by the nature of their condition. All the other areas measured by the health concepts in the SF – 36 showed, improvements bringing them within the norm for their age group and sex.
Client 2. At the time this client carried out the post-CAT evaluations, they had just been told that, before a long-awaited medical procedure could take place, they needed to undertake further physical rehabilitation. This caused a great deal of distress and the client isolated themselves and became low in mood. However, the client did not enact the self-destructive procedure of taking drugs or alcohol to manage their feelings, which had been their dominant coping strategy pre-brain injury. This reflects the results of the SF – 36 scores being lower for the role physical (rp), role emotional (re), social functioning (sf), mental health (mh), energy/vitality (ev) being lower. Whilst in the areas of bodily pain (p) and general health perception (ghp) there was an improvement.
Client 3. The SF – 36 scores showed that post CAT therapy this client had improved in the areas of role functioning (rf), role physical (rp), social functioning (sf), mental health (mh), energy/vitality (ev), and bodily pain (p). They reported same scores for role emotional (re), and this could be owing to the continuing financial pressure the client was under in not being able to return to paid employment at this time. Also, their additional adjustment to the new role of parent meant that they had put their energy into their role and responsibility as a parent. The lower scores of physical functioning (pf) and general health perception (ghp) can be explained by their increased insight and acceptance of their physical impairments and a more realistic view of their physical limitations following therapy. This client also had the additional role change of being a new parent which made their rehabilitation more complex and demanding.
Clients 2 and 3 did not attend owing to further medical treatment and family and financial crisis. The CAT practitioner and clients believed therapy helped them to not enact unhelpful procedures such as using drugs and alcohol to manage feelings or dismiss and deny their own difficulties and attempt to cope alone.
My reflections
The three ABI CAT clients with whom I worked had experienced positive relationships and had achieved great success in their work roles and life prior to their brain injury. They all showed a strong commitment to work in therapy and in their community rehabilitation. They were all high achievers in their work/vocational choice areas. I don’t expect they were people who would have come to therapy if they had not had a brain injury. Only one client had a self-damaging procedure of using drugs and alcohol as a way of coping with their low mood prior to their injury. The initial feedback from the clients was that I should make more explicit why I was asking about their life and relationships prior to their injury, as it only became clear why this was important at the Reformulation stage of therapy and was very different to the sorts of information asked of them by other members of the treating team.
It was very easy to form a working alliance with all three clients as they were highly motivated - not to say desperate - to feel better and “get their life back”. Any initial reservations I had about whether the CAT model would be beneficial to my clients was dispelled as soon as they began to make progress. In particular, the first client started making significant changes midway through the therapy. This work was and still is rewarding, exhilarating, moving and distressing, sometimes all at the same time. All three of the clients felt they had got a long way towards getting what they needed from the therapy. One described CAT as “the perfect thing at the right time”.
On reflection, perhaps the reason why the “striving” procedure stood out as such a key coping strategy in all three clients is because, prior to suffering an ABI, it is a very successful procedure for helping people achieve success and reach their goals. Striving, perfectionism and performing at a high level are beneficial in many if not all areas of working life. However, as mentioned above, they are at odds with recovery from brain injury and in particular with managing fatigue symptoms.
All three clients made significant life changes and adjusted to the residual impairments that their brain injury imposed upon them. They also were able to adjust to the associated medical conditions which had either caused their injury or happened at the same time as they sustained it. The outcome measures do not do justice to these achievements in their lives and the lives of their families. They have inspired the team to make CAT a small but significant part of our community brain injury rehabilitation service.
Supervisor’s Reflections
The introduction of Cognitive Analytic Therapy to the service for those with Acquired Brain Injury represented a new experience for both Supervisor and Practitioner. Whilst we were both willing and ready for the challenge, it was important from my position as a supervisor that certain conditions were in place before risking a new intervention with this client group. This included a written contract for supervision arrangements from the appropriate manager. This enabled Caroline and I to put our faith into the model and collaborate together with the project.
It was important to adhere to the model as this was our common ground and gave us consistency. I had no direct experience of working with this client group and we paid particular attention to the formulation of presenting problems before committing to the offer of CAT. I believe this was containing for us both and therefore containing for the clients. This client group present with particular challenges and the use of the CAT tools acted as a container for both client and therapist. We experienced the ‘parallel process’ of feeling the demand of new challenge but also the reward of involvement in a stimulating new experience. It has enhanced our faith in the model, and within our Trust CAT is now available to a client group who cannot usually gain access to the valuable experience of CAT.
Maria Ozanne, Nurse Specialist, CAT Supervisor, Intensive Psychological Therapies Service, Dorset Healthcare University Foundation Trust.
Conclusions:
A standard 16 session CAT appears to be an effective individual psychological intervention with clients with mild and moderate acquired brain injury. All the clients attended for follow-up but only one client was able to attend for all three of the scheduled follow-up sessions at one month post therapy, three months and finally six months post therapy. Their outcome measures and feedback from clients at their follow up appointments suggests that their improvement was maintained and improved upon post CAT.
It may be that clients with moderate ABI would benefit from and have better outcomes from, a longer than standard CAT. Coetzer (2008) in his model of community-based neuro-rehabilitation suggests that input from brain injury professionals should be over a longer period of time in order for problems of identity change to occur, because difficulties of this nature seem to require longer term work. This would be in line with the longer therapy of 24 sessions with clients with a diagnosis of Borderline Personality Disorder (BDP) and the longer therapies of clients with Learning Disabilities (LD). All the CAT clients attended for follow up appointments and two of the three have been discharged from the community brain injury service with positive outcomes. The third client has had to adjust to the additional role of being a parent, as well as dealing with their own recovery and vocational rehabilitation and they too are continuing to achieve positive outcomes in their life and recovery from ABI.
Further work:
As the number of clients with a mild to moderate ABI and receiving a CAT increases (six to date), the data collected from the outcome measures will reach a sample size which will allow further statistical analysis.
One of the observed clinical outcomes of the CAT appeared to be clients’ improved “emotional processing”. Our clients appeared to show improvements in their cognition as well as emotional distress and psychological functioning during and as a result of the CAT. Roger Baker (2007) has generously allowed us to use his Emotional Processing Scale (EPS) pre-and post-CAT to look at changes in emotional processing following therapy and to aid the reformulation process of CAT to include an emotional processing style.
Evidence of a “striving” procedure in clients recovering from mild and moderate ABI and difficulty in accepting professional advice to “pace yourself” are being identified as factors by which clients may be prioritized for interventions based on the underlying management of their feelings, rather than only standard education and advice on managing fatigue.
There is scope for using CAT in the community brain injury service in other ways than as an individual therapy with clients, in the same way that mental health clients in community mental health teams may not be able to benefit from CAT, but their staff team may benefit from a formulated care plan approach similar to that described by Dunn and Parry (1997). A similar team approach could be beneficial in CBIS. Clients with severe ABI who would not be able to use individual CAT due to the severity of their brain injury but who have behavior problems such as the ones described by (Yeates et al. 2008) may put themselves at risk by rejecting the home care or rehabilitation they need. A CAT formulation directed at their paid carers may be beneficial in these circumstances.
There may also be scope for offering CAT to the partner/spouse or parent of the severely brain injured patients who live at home with their family having CAT in order for the family member to revise the coping strategies which may prevent them and the person with the brain injury getting the help and support they need.
Acknowledgements:
To the three clients who bravely engaged without reservation in their therapy, for without out their hard work and determination to recover from their injuries none of this would be possible.
To Dr Birgit Gurr, Clinical Neuropsychologist, for encouraging me to work using CAT with her client with an acquired brain injury.
To all my colleagues in the Community Brain Injury Service at Dorset Healthcare University Foundation Trust for their support and interest in this work.
Special thanks to Maria Ozanne, CAT Clinical Supervisor: none of this would have been possible without her knowledge and expertise in a new area of CAT practice.
Also, thanks to Hannah Whitney, Emma Selwood and especially Laura Merrett for help with the proposal, research design and analysis of data in this study.
To Christopher Rice for all his support, encouragement and the shaping of this paper, to William Rice for creating the SDR diagram and to Elizabeth Rice for putting up with my CAT pre-occupation.
Liana Murphy for her valuable and timely support with the final draft.
Affiliations
Caroline Rice-Varian, Clinical Specialist Occupational Therapist Community Brain Injury Service, Dorset Healthcare University Foundation Trust. I trained in CAT on the Dorset Practitioner Course from 2004 – 2006.
Address
Caroline Rice-Varian, Community Brain Injury Service, Dorset Healthcare University Foundation Trust, Poole Community Health Clinic, Shaftesbury Road, Poole, Dorset, BH15 2NT. caroline.rice-varian@dhuft.nhs.uk
Appendix: Results
Quantitative measures. The Statistical Package for the Social Sciences Version 14 (SPSS 14) was used to look at the scores of the three clients. Only descriptive analysis was used, owing to the small sample size.
Hospital Anxiety and Depression Scale (HADS) norms:
0-7 Normal; 8-10 Borderline Abnormal; 11-21 abnormal
SF-36 (Short Form 36 health survey questionnaire) includes eight scales:
1) physical functioning (pf), 2) role limitations due to physical health problems (rp); 3) role limitations due to emotional problems (re), 4) social functioning (sf), 5) mental health (mh), 6) energy/vitality (ev), 7) bodily pain (p), 8) general health perception (ghp).
On all of these scales, the higher the score the better the level of functioning.
Client 1
HAD scores before CAT: Anxiety 9, Depression 8; after CAT: Anxiety 4, Depression 1 (i.e. both Anxiety and Depression within normal ranges)
CORE global score pre-CAT was 50 (Mild level of distress band) and post CAT 4 (Healthy).
SF-36. After CAT, 7 of the 8 scales showed increases (i.e. improvement). See discussion.
Client 2
HAD scores before CAT: Anxiety 12, Depression 8; after CAT: Anxiety 9, Depression 6 (i.e. Anxiety changed from abnormal to borderline, and Depression from borderline to normal)
CORE global score pre-CAT was 67 (Moderate level of distress band) and post CAT 59 (still within the Moderate level of distress band, but 8 points lower).
SF-36. After CAT, improvement in functioning in three areas; the physical functioning (pf), bodily pain (p) and general health perception (ghp). This client scored lower in role physical (rp), social functioning (sf), mental health (mh), energy/vitality (ev). And the same for role emotional (re). See discussion.
Client 3
HAD scores before CAT: Anxiety 15, Depression 9; after CAT: Anxiety 12, Depression 7 (i.e. Anxiety changed from abnormal to borderline, and Depression from borderline to normal)
CORE global score pre-CAT was 51 (Moderate level of distress band) and post-CAT 44 (Mild level of distress band).
SF-36. After CAT, improvement in functioning in six of the eight scales. See discussion.
References:
Anderson, C., Laubscher, S., Burns, R., (1996) Validation of the Short Form 36 (SF-36) Health Survey Questionnaire among stroke patients. Stroke. Vol. 27., No. 10. October 1996.
Baker, R. (2007) Emotional Processing. Lion Hudson.
Cluley, S., Smeeton, N., Cochrane, G. M., and Cordon, Z. (2000) The use of cognitive analytic therapy to improve adherence in asthma. (Submission)
Coetzer, R. (2008) Holistic Rehabilitation in the community: is identity the issue? Neuropsychol Rehabil. 2008 Oct-Dec 18 (5-6):766-83.
Connell, J., Barkham, M., Stiles, W. B., Twigg, E., Singleton, N., Evans, O., Miles, J. N. V., (2007) Distribution of CORE-OM scores in a general population, clinical cut-off points and comparison with CIS-R. British Journal of Psychiatry (2007). 190, 69-74.
CORE Partnership (2007) Is initial overall CORE-EM score an indicator of likely outcome? CORE Partnership Occasional Paper, No. 1. CORE IMS: Rugby.
Fosbury, J. A. (1994b) Cognitive Analytic Therapy with poorly controlled type 1 insulin dependent diabetic patients. In: Coles, C. (Ed) Psychology & Diabetes Care Chichester, PMH Production.
Gilbert, P. (2010) Compassion Focussed Therapy Routledge.
Gilbert, P. (2009) The Compassionate Mind Constable & Robinson.
Gracey, F., Evans, J.J, Malley D., (2009) Capturing outcome in complex rehabilitation interventions: A “Y” shaped model. Neuropsychol Rehabil. 2009 Dec. 19(6):867-90. Epub 2009 Jul 16.
Jellema, A., Crowley, V., Griffiths, T., Twist, G., Gray, S. (2003) Developing and Promoting CAT in the NHS. Problems and Possibilities. Reformulation 2003
Johnston, M., Pollard, B., Hennessey, P., (2000) Construct validation of the hospital anxiety and depression scale with clinical populations. Journal of Psychosomatic Research 48 (2000) 579-584.
King, R. (2005) CAT. The Therapeutic Relationship and Working with People with Learning Disabilities. Reformulation Issue 24, 2005.
Nehmad, A. (2010) A CAT Perspective on Theorizing, Eliciting and Strengthening the Healthy Self. ACAT Conference July 2010.
Nehmad, A. (1997) The Essence of Effective Psychotherapy. Reflections of a CAT Therapist learning Solution Focussed Brief Therapy. Reformulation
Malia K & Brannagan A (2007). Hero’s Journey Brain Tree Training, UK
McCormick, E. Wilde (2008) Change for the Better. 3rd Ed. SAGE Publications.
Powell, T. (2004) Head Injury: A Practical Guide (Speechmark Editions)
Quraishi, M. (2009) CAT Effectiveness: A Summary. Reformulation Summer 2009.
Ryle, A. & Fonagy, P. (1994) Psychoanalysis, Cognitive Analytic Therapy, Mind and Self. BJP Annual Lecture 1994. British Journal of Psychotherapy 11, 4, 567-574.
Ryle, A, Golynkina, K. (2000) Effectiveness of Time-Limited Cognitive Analytic Therapy of Borderline Personality Disorder: Factors Associated with Outcome. British Journal of Medical Psychology (2000), 73, 197 – 210.
Ryle, A., & Kerr, I. (2002) Introducing Cognitive Analytic Therapy. Principles and Practice. Wiley.
Yeates, G., Hamill, M., Sutton, L., Psalia, K., Gracey, G., Mohamed, S., & O’Del, J. (2008) Dysexecutive Problems and Interpersonal Relating Following Frontal Brain Injury: Reformulation and Compensation in Cognitive Analytic Therapy (CAT). Neuro-Psychoanalysis, 2008, 10 (1).
Ware, J.E.,Jr., Kosinski, M., Gandek, B. SF-36 Health Survey: Manual & Interpretation Guide. Lincoln, RI: QualityMetric Inc., 1993, 2000.
Wells, S. (2009) A Qualitative Study of Cognitive Analytic Therapy as Experienced by Clients with Learning Disabilities. Reformulation Issue 33. 2009.
Zigmond, A. S., & Snaith, R. P., (1983) The Hospital Anxiety and Depression Scale. Acta Psychiatry Scand. 1983: 67: 361-370.
 Petition to NHS England - The Case for Funding Training in the NHS 2021
Alert!
Petition to NHS England - The Case for Funding Training in the NHS 2021
Alert!ACAT's online payment system has been updated - click for more information

Full Reference
Rice-Varian, C., 2011. The Effectiveness of Standard Cognitive Analytic Therapy (CAT) with people with mild and moderate acquired brain injury (ABI): an outcome evaluation.. Reformulation, Summer, pp.49-54.Search the Bibliography
Type in your search terms. If you want to search for results that match ALL of your keywords you can list them with commas between them; e.g., "borderline,adolescent", which will bring back results that have BOTH keywords mentioned in the title or author data.
Related Articles
Applying CAT in an Acquired Brain Injury Neuropsychology service: Challenges and Reflections
Calvert, P., 2014. Applying CAT in an Acquired Brain Injury Neuropsychology service: Challenges and Reflections. Reformulation, Summer, pp.16-21.
CAT Effectiveness: A Summary
Quraishi, M., 2009. CAT Effectiveness: A Summary. Reformulation, Summer, pp.36-38.
Evaluation of CAT in GP Practice
Baker, J., 2003. Evaluation of CAT in GP Practice. Reformulation, Spring, pp.16-17.
The CAT Articles Review
Knight, A., 2009. The CAT Articles Review. Reformulation, Summer, p.32.
An audit of Goodbye Letters written by clients in Cognitive Analytic Therapy
McCombie, C., Petit, A., 2011. An audit of Goodbye Letters written by clients in Cognitive Analytic Therapy. Reformulation, Summer, pp.42-45.
Other Articles in the Same Issue
Aim and Scope of Reformulation
Hepple, J., Lloyd, J., Shea, C., 2011. Aim and Scope of Reformulation. Reformulation, Summer, p.56.
An audit of Goodbye Letters written by clients in Cognitive Analytic Therapy
McCombie, C., Petit, A., 2011. An audit of Goodbye Letters written by clients in Cognitive Analytic Therapy. Reformulation, Summer, pp.42-45.
Book Review: Lacanian Psychoanalysis, Revolutions in Subjectivity
Pollard, R., 2011. Book Review: Lacanian Psychoanalysis, Revolutions in Subjectivity. Reformulation, Summer, pp.23-28.
Book Review: The Mindfulness Manifesto
Wilde McCormick, E., 2011. Book Review: The Mindfulness Manifesto. Reformulation, Summer, p.28.
CAT, Metaphor and Pictures: An exploration of the views of CAT therapists into the use of metaphor and pictorial metaphor
Turner, J., 2011. CAT, Metaphor and Pictures: An exploration of the views of CAT therapists into the use of metaphor and pictorial metaphor. Reformulation, Summer, pp.37-41.
Dear Reformulation
Hughes, R., 2011. Dear Reformulation. Reformulation, Summer, p.22.
Flowers by the Window: Imagining Moments in a Culturally and Politically Reflective CAT
Brown, R., 2011. Flowers by the Window: Imagining Moments in a Culturally and Politically Reflective CAT. Reformulation, Summer, pp.6-8.
Is CAT in danger of being squeezed out of the NHS?
Waft, Y., 2011. Is CAT in danger of being squeezed out of the NHS?. Reformulation, Summer, pp.18-21.
Is three a crowd or not? Working with Interpreters in CAT
Emilion, J., 2011. Is three a crowd or not? Working with Interpreters in CAT. Reformulation, Summer, p.9.
Letter from the Chair of ACAT
Hepple, J., 2011. Letter from the Chair of ACAT. Reformulation, Summer, pp.4-5.
Letter from the Editors
Hepple, J., Lloyd, J. and Shea, C., 2011. Letter from the Editors. Reformulation, Summer, p.3.
Memoirs, Myths and Movies: Using Books & Film in Cognitive Analytic Therapy
Jefferis, S., 2011. Memoirs, Myths and Movies: Using Books & Film in Cognitive Analytic Therapy. Reformulation, Summer, pp.29-33.
Six-Part Storymaking – a tool for CAT practitioners
Dent-Brown, K., 2011. Six-Part Storymaking – a tool for CAT practitioners. Reformulation, Summer, pp.34-36.
The Effectiveness of Standard Cognitive Analytic Therapy (CAT) with people with mild and moderate acquired brain injury (ABI): an outcome evaluation.
Rice-Varian, C., 2011. The Effectiveness of Standard Cognitive Analytic Therapy (CAT) with people with mild and moderate acquired brain injury (ABI): an outcome evaluation.. Reformulation, Summer, pp.49-54.
The Reformulation '16 plus one' Interview
Hepple, J., 2011. The Reformulation '16 plus one' Interview. Reformulation, Summer, p.55.
Using a template to draw diagrams in Cognitive Analytic Therapy
Jenaway, Dr. A. and Rattigan, N., 2011. Using a template to draw diagrams in Cognitive Analytic Therapy. Reformulation, Summer, pp.46-48.
What are the most dominant Reciprocal Roles in our society?
Ahmadi, J., 2011. What are the most dominant Reciprocal Roles in our society?. Reformulation, Summer, pp.13-17.
Help
This site has recently been updated to be Mobile Friendly. We are working through the pages to check everything is working properly. If you spot a problem please email support@acat.me.uk and we'll look into it. Thank you.
