What is the 2005 Mental Capacity Act and how can CAT help us to make sense of the decision making process at its heart?
Brown, H. and Lloyd, L., 2012. What is the 2005 Mental Capacity Act and how can CAT help us to make sense of the decision making process at its heart?. Reformulation, Summer, pp.35-42.
Mental capacity is a key concept in health and social care services and provides one important mandate for the interventions of professionals and welfare services. In parallel with the Mental Health Act, the 2005 Mental Capacity Act (MCA) defines when a professional can step into another person’s life and take control of certain areas of decision making, enforcing actions that the person might otherwise refuse. There are therefore major human rights issues about its application and about the rights of vulnerable individuals to challenge decisions made by others who are purporting to act “in their best interests”. The workings of individual practitioners within the MCA have to be defensible, impartial, transparent and open to appeal.
Because this was such an important, and long-awaited piece of legislation, there was a long consultation period before its passage into law in 2005 and its implementation in April 2007. A series of reports were produced during the 90’s so that key areas of controversy had been widely debated, for example the relative advantages of different forms of proxy decision making e.g. next friend, or substitute decision-making, as opposed to the test of “best interests” decision-making that was finally adopted. An impressive array of agencies and advocacy groups supported the Bill as it went forward and there was widespread support for its principled and streamlined model of decision-making.
The legislation, and the principles it sets out, are key to practice in learning disability services and services for older people. It is also relevant in relation to eating disorders and autism. As therapists we need to understand it in case we need to invoke it in our own practice but also our CAT understanding helps us to think about some of the tensions within the MCA, its principles and the model of decision-making at its core. So in this paper we begin by exploring the MCA and then move on to use a number of key psychological and CAT concepts to “test” its model, suggesting why “one size” does not necessarily “fit all” when it comes to making decisions.
Background to the MCA
The MCA was welcomed because it filled a vacuum. Before it was introduced only a few precepts of common law allowed one person to step in and act on behalf of someone who was not able to make their own decisions. This led to strange anomalies; emergency treatment could be offered but not elective or well planned care; some carers had no official way of appropriately taking charge of aspects of their relative’s care, while others took too much control of matters that individuals would have been able to manage, with assistance, on their own.
People were deemed to lack capacity in all areas of their lives, or to have it across the whole span of their activities. This situation was replaced by a commitment to assess the person’s ability to make each and every decision, in a rational way which clarifies and structures assessment and intervention but that also seems to deny important psychological understandings and relational realities.
Life rarely presents in terms of clear well-formulated “decisions”. Some clients tend to find it hard to act on their own behalf in multiple ways. Setbacks lead people to recoil from decision-making until they live in a muddle and no one is sure whether they should or could intervene. Others run risks that seem irrational, or limit their choices because they are overly sensitive or reactive. Black and white notions of “choice” and “rights” obscure the fact that, in the words of a recent serious case review “Most people do not, at some clear point in their lives, choose to live in squalor and danger. (Scourfield 2010).
The present paper seeks to find a middle ground, upholding the MCA’s strengthening of the human rights of vulnerable people while challenging, and elaborating on, its decision making model. So as CAT therapists we both need to use the Act and we can also inform others about its use adding our relational ideas into the mix of professional debate and good-enough practice.
The Mental Capacity Act 2005
The Mental Capacity Act 2005 (MCA) provides a statutory framework to empower and protect vulnerable people who are not able to make their own decisions. It makes it clear who can take decisions, on behalf of another person, in what situations, and what principles they should apply.
The MCA has a number of components.
- Firstly, it sets out a set of principles to guide people who are assessing capacity and/or making decisions on behalf of others.
- Secondly, it sets out a decision-specific definition of capacity and a test for assessing whether a person can, at a given time, and with appropriate information, make this decision for themselves.
- Thirdly, it provides a range of instruments that people can use to state their intentions in advance and designate who they wish to administer their affairs and act for them in making welfare decisions, at a future time when they may lack capacity: this they can do through granting a Lasting Power of Attorney in advance of any difficulties and if they have not done so the Court can appoint a Deputy retrospectively.
Mostly the MCA tries to set up a do-it-yourself model that allows sensible decisions to be made by those closest to the person and most involved in putting them into operation. Only highly complex, serious or contentious cases are subject to court hearings.
Once it has been decided that a person is not able to make a decision for themselves then the person deemed appropriate to act on their behalf has to do so “in their best interests” which is not the same as ‘doing what they say they want.’ so it can lead to situations where one person, albeit responsibly, is forcing another down a particular route. This is a position that health and social care workers find uncomfortable and often they go on trying to persuade and cajole, when the responsibility for what is to be done has passed into their hands.
Upfront the MCA states five core principles; the first three enshrine a person’s right to make decisions for themselves unless it can be shown that they are unable to do this for themselves and the last two set out the essential guidance for anyone acting on behalf of someone they have assessed as lacking capacity.
- A presumption of capacity - every adult has the right to make his or her own decisions and must be assumed to have capacity to do so unless it is proved otherwise.
- The right for individuals to be supported to make their own decisions - people must be given all appropriate help before anyone concludes that they cannot make their own decisions.
- That individuals must retain the right to make what might be seen as eccentric or unwise decisions.
- Best interests – anything done for or on behalf of people without capacity must be in their best interests and
- Least restrictive intervention – anything done for or on behalf of people without capacity should be the least restrictive of their basic rights and freedoms.
This framework allows most issues to be resolved by the person and their immediate circle, and, in general, formal arrangements or hearings are avoided. The MCA is administered by the Office of the Public Guardian and adjudicated by the Court of Protection. The Court is brought in only when
- there is a dispute around a finding of incapacity:
- there is disagreement between family members, carers and/or professionals as to the person’s capacity:
- the person concerned is expressing different views to different people, perhaps through trying to please each or tell them what s/he thinks they want to hear:
- the person’s capacity to make a particular decision may be subject to challenge, either at the time the decision is made or in the future:
- there may be legal consequences as a result of a finding of in/capacity:
- the person concerned is repeatedly making decisions that put him/her at risk or that result in preventable suffering or damage.
So the Court’s intervention is not needed for day-to-day decision-making or management of a person’s affairs and “informal” carers are allowed to do what is needed unless things are complex, irreversible (such as sterilization) and/or contentious and disputed.
How is “Mental Capacity” defined in the MCA?
The MCA sets out a two-stage test of whether a person lacks capacity - the first part is more diagnostic and establishes that there are grounds to hold concerns about the person’s mental capacity and the second part is "decision-specific" and time-bound , hence you need to ask
1. Does the person have an impairment of, or a disturbance in, the functioning of, their mind or brain?
This is the only “global” part of the test that may specifically fall to a psychiatrist or psychologist to diagnose: otherwise the “decision-maker” is the person responsible for making a judgment about the specific aspect of the person’s care under consideration. Therapists concerned about sharing information, for example, should not look to medics to make decisions for someone about confidentiality or disclosure. If in their judgment, the person is not able to weigh up the pros and cons for themselves, at that time, then it is for them to make the decision in their client’s best interests.
The MCA makes it very clear that you cannot infer a lack of capacity based on a person’s medical condition or diagnosis alone, or by reference to a person's age, appearance, intellectual level or any condition or aspect of a person's behavior, which might lead others to make unjustified assumptions. Nor do you have to establish whether their incapacity is permanent or temporary so the second more specific question to ask is
2. Does the impairment or disturbance mean that the person is unable to make a specific decision when they need to?
The assessor is charged with making the necessary information accessible to the person if at all possible and then has to ask in relation to “the matter at hand” whether the person is able to
A. to understand the information relevant to the decision,
B. to retain that information,
C. to use or weigh that information as part of the process of making the decision, and/or
D. to communicate his decision (whether by talking, using sign language or any other means).
User groups were pleased with the assumption of capacity which places the onus on the carer or professional to show the person lacks capacity rather than on the person to demonstrate their competence.
The “test” of capacity was deliberately set low to ensure that there was a “hands off” ethos wherever possible.
For example, Mr Justice Hedley, deliberating on the capacity to understand sexual relationships spoke of a level that would be “very modest not really going beyond an awareness of ‘right’ and ‘wrong’ behaviour as factors in making a choice” augmented by “rudimentary” knowledge of sexual health and an emotional component that is boiled down to “does the person whose capacity is in question understand that they do have a choice and they can refuse?(1).” The person only needs to be able to retain the information in their memory for as long as needed to make the decision.
The model of decision-making that is taken as the norm in the MCA, is that of a rational, independent person “choosing” from an appropriate range of options, on the basis of sufficient and salient information. The focus is on information processing, i.e., a cognitive model looking at access to information, comprehension, memory, executive functioning and communication. These functions are not named in the MCA but for example ‘executive functioning’ is wrapped up in the person’s ability to weigh up the relevant issues. The threshold of proof required in the MCA is “on the balance of probabilities” and this recognizes that in some of these situations the person’s capacity cannot ever truly be known.
So this is a clear and focused framework but one based on a cognitive, linear model of decision-making, that does not take emotional stability or relational patterns into account and it is here that the model can falter.
It is as if the people and issues requiring attention lie on a continuum. At one end the decisions to be made are clear-cut; a person has capacity and is choosing to do or not do something, and the professional rightly has to limit their intervention to informing, supporting and persuading. At the other end of the spectrum the way forward is also clear cut in that the person does not have capacity and demonstrates pervasive difficulty in making decisions so that everyone in the family and professional network is clear that it is their responsibility to act on the person’s behalf. There may be contention about what is in the person’s best interests, but the locus of the responsibility is not in dispute. But it is in the middle ground that the issues are more complex: there may be contention about both who decides and about what is to be done. And there is a difficult tipping point where the professionals who have been attempting to support the person have to switch into a more authoritative role in order to act responsibly on behalf of the person even when this is not what they appear to want.
A wide range of decisions and circumstances
So how do these issues get reflected in the life of a busy health care professional in the real world of Health and Social Care services? The MCA was designed to address one-off serious decisions, specifically those relating to serious medical treatment and to changes of accommodation but in fact we find it necessary to apply the MCA in relation to a much broader range of decision-making that is more likely to be ongoing. So for example the framework within the MCA sits much more easily alongside a decision about cancer treatment than ongoing management of diabetes.
The authors both regularly receive referrals or have to consider cases where it has to be stretched to fit the reality of people’s day-to-day lives. The first author conducts reviews of safeguarding interventions where decisions have been made against a backdrop of abuse or neglect and the second author, working as a clinical psychologist in a service for people with learning disability, is regularly asked to make capacity assessments in relation to complex situations where an understanding of reciprocal roles is at least as important as an understanding of the person’s cognitive processing abilities.
The kinds of cases and decisions that result in such referrals have included assessing issues around marriage, including whether to stay in potentially abusive relationships, sexuality, including when taking risks, staying in or leaving the parental home, signing over property or giving away money, setting up a power of attorney, working without pay in a context that could be seen as exploitative, eating a very restrictive diet, managing aggressive behavior or stealing that is potentially criminal. Often the subtext of a referral is quite punitive, and formulated as “is this person responsible for what they are doing, if so we will back off and let them take the consequences.”
At times there is an important role switch that has to be made from collaboration to taking control that is perhaps similar to situations in which a therapist has to make a formal safeguarding alert, or a psychiatrist has to detain someone under the Mental Health Act. Shifting from a facilitative mode into an authority figure is uncomfortable and requires confidence. Supervision from informed supervisors is one of the tools we have to help us, as practitioners, to navigate such switches.
It is in these complex situations that the MCA’s core principles, structure for assessment and clarity about best interests as the basis for any substitute decision-making, come to the fore.
Applying the MCA in complex cases
Moreover the issues rarely present themselves in a clear order or package. Within the MCA and its accompanying guidance, there is an assumption that there will be a single, one-off, boundaried decision rather than a series of muddled, small but cumulatively damaging decision-making over time. Often the proposed intervention comes at the end of a long road of difficulties and compromises, when options are limited and time is in danger of running out.
A recent study (Brown and Marchant 2011) of cases deemed complex by health and social care professionals illustrated the components of a case that made these matters problematical. This study explored the factors that led practitioners to define a case as complex at different stages of the process. The cases they submitted to the research project suggested that complexity could be inferred where
- there was a spiraling set of inter-related concerns and no clear trigger that put a single well formulated and boundaried “matter” on the table:
- the person’s capacity was at issue in a number of ways, they may have been inconsistent but articulate in what they wanted, vociferous (especially in refusing services) but not informed, or they may have reacted rather than decided around important things suggesting to us that the person may have been triggered into different mental states from which contradictory decision-making could be expected and made sense of:
- a person’s ability to separate out information from emotional responses, addiction or neurological drives was in question; So, for example, one woman would not let a carer into her house to change her incontinence pad because she had a fear of social workers dating back 30 years when they had been involved in a more controlling role in relation to her children. Here we saw her as being triggered into a controlling to controlled reciprocal role that overrode her need to get looked after in this most basic and immediate way:
- the person’s capacity for retaining pertinent facts and for conceiving of alternatives to their current situation was compromised. Social workers spoke about people getting stuck on the “mythical option” and not being able to even think about the things that were possible: CAT therapists might see this in terms of the top half of the split egg, where the idealized trumps the real and blocks compromises. Sometimes this means that someone will reiterate that they want to “go home” or to be cared for by a loved relative, even when that person is saying they can’t do what they are being asked to do:
- in situations where the decisions were more like dilemmas than choices, and revolved around relationship and belonging, not information, risks and consequences. For example, they might present as family ultimatums of the “you can choose your boyfriend or stay part of this family” kind:
- when the Court of Protection stepped in, often after large damages awards in respect of catastrophic injury, the money complicated rather than mediated family dynamics: so, for example, it was not enough to stop a family whose style of relating was conflictual, from arguing or, if arrangements were predicated on one partner having taken on an idealized caring role in relation to a partner’s sudden onset of disability, this did not preclude the carer from eventually moving on and finding themselves in new relationships or with new priorities:
It seemed, from the 57 cases submitted to this project, that relationship and reciprocal roles provided a clearer window onto what was happening than the information-processing model of decision-making that the MCA sets out. The cognitive, linear template seemed not to describe the real world in these cases, but instead drove a Roman Road across what was actually an undulating landcape.
We should not be surprised about this primacy of emotion and relationship as psychological research has long established the role of emotion and heuristics in decision making (Brown 2012). Damasio’s series of studies (2010) showed that where a person has brain lesions that block access to emotions the person is also unable to make decisions because emotion helps us to prioritise salient information and because it drives our intentionality and motivates us in acting on and implementing decisions we have made.
Nor, as CAT therapists, are we surprised at inconsistency as we anticipate shifts in mental state as a contributory factor to complexity. Furthermore, not only are our emotional states fragmentary, but our cognitive processing is specific to those states, and our recall of memory in those states is distinct and contradictory. The trigger- happy thinking we see in highly reactive reciprocal roles does not bother to add up the itemized bill but rushes to the bottom line. Meanwhile, withdrawn and more avoidant states inhibit our thinking and cut across active seeking out of options so that our horizons close in.
Kahneman (2011) sets out the evidence base for there being two distinct systems of thinking; a “fast” and a “slow” mode of operating. The former is intuitive, emotional and jumps to conclusions, taking what are usually helpful shortcuts. The latter is more computational, requires concentration and can inhibit or steer the more impulsive and driven qualities of the former. In CAT terms we might think of “fast” thinking as the assumptions we make on the basis of habitual reciprocal roles and procedures which, while absorbed from our experiences, can often escape rational scrutiny until we engage a more questioning, reflective stance.
Kahneman states that “emotion now looms much larger in our understanding of intuitive judgments and choices than it did in the past” (2011, p120). He also argues that what we see as the learning encapsulated in reciprocal roles is embodied, in that “you think with your body, not only with your brain” (op cit p51). That is why in CAT we write a narrative but also produce an overview and work with enactments in the relationship as it is manifest “in the room”.
What can CAT tell us about the limitations to this model?
So as CAT therapists we expect to see people occupying different mental states with varying degrees of integration and organization. We think of people as a bundle of selves and recognize /expect inconsistency as people move in and out of different, sometimes contradictory and/or intense self-states. For clients with very painful or unworked through procedures, decision making is hampered in the ways we describe in CAT as dilemmas, that is not having enough options to consider; traps, that is trying to avoid certain outcomes but cutting off our noses to spite our faces, or snags, which involve us trimming our sails in case we steal anyone else’s wind.
This suggests the need for assessments that contextualize decision-making in terms of history and relationship. It hints at other important measures of capacity such as how stable the person is, how open-minded the person is when canvassing options and how far they are able to act on their understanding to put options and choices into operation. It is interesting that in recent legal thinking about when to acknowledge a person’s wish for assisted suicide the phrase that is used is that the person should have a “fixed and stable” wish to die, not a fleeting despair or depression.
People with borderline/emotional intensity conditions are more likely than other people to make decisions that are contradictory, or that have the quality of knee-jerk reactions rather than thought through deliberations. They may have powerful splits that are reflected in decisions that come to be labelled by exasperated others as manipulative.
For example one woman with learning disability and borderline personality disorder in one of our services spent much time involved in demanding a doctor because she had been struck off by local surgeries and she had been asked to attend a special scheme. She went to enormous lengths seeking perfect care but as soon as a specific service was offered she would come up with endless reasons why the arrangement was not good enough: she refused to be seen by a man, or she took against another doctor for being older. Her objections made no sense in isolation but when her history of abuse at the hands of her mother was factored in her behavior represented her multiple fears that what she was asking for might turn out to be toxic as the care her mother had given her had proved to be. She was like Snow White being offered a poisoned apple when she craved for a sweet and crisp apple like those offered to her siblings.
This cycle cut across this client’s mental capacity in relation to her health care not because she did not “understand” at a cognitive level that she needed medical treatment but because at the height of this procedure she was not able to think about her actual health care needs and how to get them met in a timely way at all.
The research on complexity also identified the difficulties posed by addiction and by self states that are tightly bound up with and or over-ridden by, physical and neurological triggers. For example a person with Prader-Willi syndrome may understand nutrition but not be able to use this knowledge to manage their pressing need to eat. As Holland and Wong (2012, p233) state, “At its most basic it is not simply an issue of understanding, it is one of control.” Acting on our decisions is therefore another step in an already complex chain reaction. For example, a man with Down’s Syndrome and Diabetes was able to differentiate healthy foods during an educational session with a community nurse but on leaving the building, he headed for the nearest sweet shop. This elicited punitive responses from staff who had taken his earlier compliance at face value. Frustrated and powerless, they assumed that he was acting defiantly and that he knew exactly what he was doing rather than interpreting his behavior as indicative of a state shift. They could hide behind the notion that he has full capacity in relation to this arena of decision-making even though acting on the nutritional information he had been given was way beyond his zone of proximal development (ZPD). Vygotsky’s often-quoted and useful definition of ZPD is:
“the distance between the actual developmental level as determined by independent problem solving and the level of potential development as determined through problem solving under adult guidance, or collaboration with more capable peers.” (1978, p86).
CAT’s relational understanding might formulate this as a sequence of unhelpful reciprocal roles; starting with a compliant and pleasing role in response to a concerned, benevolently controlling one, moving into a more needy/ abandoned position in which the client seeks immediate comfort, which is perceived as him being defiant which in turn meets with dismissive and punitive responses from staff. The client’s shifting states are much more reflective of instant attempts to elicit or maintain relationship and to manage feelings than of planned or “deliberate” choices.
Ryle (1995), describes how if a person’s attempt at exacting reciprocation fails, they will shift to another state rather than revise how they go about trying to get the reciprocation they want. This means the man with diabetes makes his decision without the previous information being held in mind. However, when seen for a follow up appointment, we may speculate he might be able to tell the nurse about healthy and forbidden foods, whilst forgetting his trips to the sweet shop. Those of us on perennial diets will recognise how these switches have little to do with having Down’s Syndrome!
Viewing decisions as Traps, Dilemmas and Snags
When decisions are seen in a CAT context, habitual reciprocal roles and procedural sequences help us to understand the limits of a person’s capacity to change and move on. We know that people without cognitive impairments also get caught in these nets and that thinking is not enough to scaffold change unless it is supported within a significant and often therapeutic relationship. As decision-makers, we all risk getting caught up in dilemmas, traps and snags.
At the stage of considering options, a person can become so bound up in polarized options that making choices becomes aversive as neither option is wanted. Often the service embeds these black and white positions in its policies and practice so for example, in relation to sexual options for people with intellectual disabilities it is
as if the client can only have the sexual freedom to have sex with whomever she chooses doing whatever act, at whatever place, at whatever time, which leads her to being abused, OR
She is kept away from sex altogether, but experiences herself as not a real woman
But this then risks becoming a trap because the client is kept away from appropriate opportunities for learning and thereby made more vulnerable to being seduced or exploited so that the services lurch between these rival options without seeking a good middle-ground where she can feel confident, take manageable risks and yet remain somewhat protected.
Traps are thereby driven by these constraints on options. CAT dilemmas are often enacted as controlling (taking over) or neglecting (doing nothing) responses to service users who lack capacity.
A typical decision maker’s trap might be:
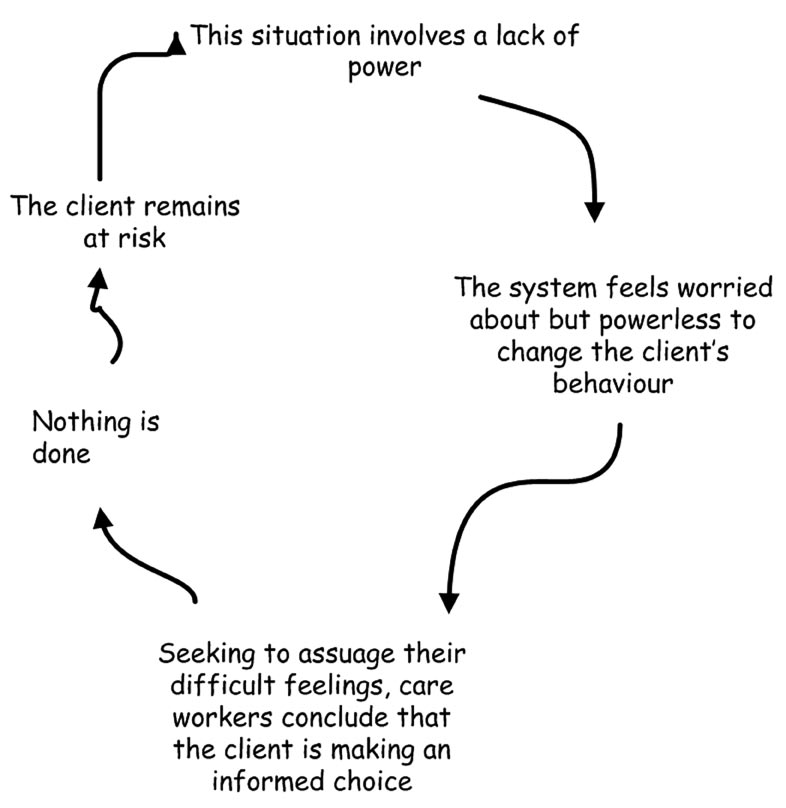
And these inconsistencies get turned into “be perfect” loops when the desire to be perfectly consistent and in control leads to system level enactments where ever more elaborate policies and guidelines are developed to anticipate all eventualities that then become unworkable and are left on the shelf. It is as if the desire to be in control leads to strategies that overwhelm and are then discarded.
Snags occur when a person’s behavior is so much under the control of others that they have no freedom to move, and this is captured in the legal formulation of “undue influence”. People who have capacity may find themselves “incapacitated” by violence, fear or control to the point where they can no longer think of options or act to bring them about. Steven Hoskin (Flynn 2011) stands as an example of this: he wanted friends but he got tormentors whom he could not stand up to. He was afraid that involvement in services would lead to old patterns of control and to him feeling different and isolated again, so he asked for help in a “scatter-gun” way and did not reveal the scale of the horrors he was facing at home or the extent to which he was being abused . Even “caring” control can undermine the attempts many people with learning disabilities make to change.
Moreover, professionals can also be caught in snags when they adjudicate in contentious issues. The expectations of other agencies, or the interpretations of fellow team members can exert a powerful influence over the way issues are framed and the role of decision-maker; for example, the role of the Approved Mental Health Professional (AMHP), contains a clear tension between reaching a consensus and acting in concert with other professionals and “taking a stand” in ways that might go against them.
People with learning disabilities and older people with dementias may find it even harder than others to correct the biases embedded in their roles and procedures, to question the efficacy of familiar strategies, to take risks by trying new things and /or to stand up to other people in their lives.
What does CAT’s collaborative stance have to offer?
One case managed by the second author involved a capacity assessment under the MCA and a subsequent best-interests decision that was submitted to a national research study (Mental Health Foundation, 2012). It involved analysis of face-to-face interviews with the CAT therapist who conducted the MCA assessment, the independent chair of the safeguarding vulnerable adults committee and the care providers. It was selected as one of two cases demonstrating exemplary practice. The CAT therapist had previously worked with the client using a CAT framework and the researchers concluded that this intervention had kept the situation out of crisis over a period of many months. The client had repeated chances to prove he had capacity and the fact that strong attempts had been made to support his decision-making were framed as additional evidence that he did indeed lack capacity. Strategies had included using accessible information and pictures to enable him to understand the risks he was facing. Contextual work with the staff team had also been very positive, and there was a trusting partnership between agencies, but in the end the situation went beyond what was possible for the care providers if they were to keep this client safe.
The CAT therapist was asked to conduct a capacity assessment when, some time after the therapy had ended, the situation dramatically deteriorated to the extent that a police investigation had ensued. The formal aspects of the chairperson’s role lent objectivity to the best interests meeting in which the meeting’s parameters were carefully stated. The client was invited to attend the second part of the best interests meeting with his advocate to give him the opportunity to work with the meeting, not against it. A large part of the resultant action plan involved careful planning and working with the client to support his safety. The researchers commented that “the skill of that meeting was at least partly the skill of enabling (the client) to have a voice and express his concerns”.
The researchers described how complex this case was and that “much depended on the particular sensitivity and skills of the psychologist, care manager and staff in the home. They felt that conflicts were avoided by this detailed level of partnership work over a period of years”.
Nuanced judgments
In deciphering these issues professionals need confidence to make nuanced judgments that are both decision-specific and that take into account the contours of the person’s relationships and history. CAT’s model of collaborative working and of recruiting healthy self-states to make sense of complexity provides a way forward when "thinking straight" has been put in jeopardy. The recruitment of healthy states is consistent with the basic assumption in the MCA of a presumption of capacity - every adult has the right to make their own decisions and must be assumed to have capacity to do so unless it is proved otherwise. But by being aware of how capacity fluctuates across different self-states and of how dilemmas, traps and snags start to operate out of awareness, we can conduct capacity assessments that more closely approximate a holistic view of real life.
Capacity assessments that take emotional as well as cognitive processes into account, can then be used to inform grounded approaches to clients and to underpin professional networks that are robust enough not to split. Consistency in the face of complex issues can then be maintained at times when individuals and teams find their ability to think is in jeopardy.
Hilary Brown and Julie Lloyd
April 2012
Hilary Brown and Julie Lloyd both work with vulnerable people; Hilary as a professor of social care at Canterbury University and in a community learning disability team, and Julie Lloyd as a clinical psychologist, also in a community learning disability team. Both are CAT therapists.
References
Brown,H. & Marchant, E. (2011). Best-interests decision making in complex cases Office of the Public Guardian London http://www.canterbury.ac.uk/social-applied-sciences/ASPD/documents/BestInterestDecisionMakinginComplexCasespaperJune2011.pdf
Brown, H. (2011). “The role of emotion in decision-making” Journal of Adult Protection vol 13 no (4), pp 194-202: Emerald Group Publishing.
Court of Protection, (2012). The Hon. Mr. Justice Hedley Judgment in relation to A Local Authority -and- H Jan 27th 2012 COP11895254
Damasio, A. (2010). Self comes to mind: Constructing the Conscious Brain, Pantheon.
Flynn, M., for Cornwall Social Services, (2011). “Serious Case Review into the death of Steven Hoskin”. http://www.google.co.uk/url?sa=t&rct=j&q=&esrc=s&source=web&cd=2&cts=1331292502299&ved=0CC8QFjAB&url=http%3A%2F%2Fwww.towerhamlets.gov.uk%2Fidoc.ashx%3Fdocid%3D1fd6e027-7ef4-4a08-bf58-e55141b79c5b%26version%3D-1&ei=UOlZT523K4q18QOzxtjaDg&usg=AFQjCNElN05ZMFffFH6FO36TqfbnqoLnyA&sig2=CVDafZ0fk2NzypN459lVaw
Holland, A., & Wong, J. (1999). “Genetically determined obesity in Prader-Willi Syndrome: the ethics and legality of treatment” Journal of Medical Ethics; 25:230-236.
Kahneman , D. (2011) Thinking, fast and slow. Clays Ltd: St Ives.
Mental Health Foundation ‘Best Interests Decisions Study’ 2012, free download http://www.mentalhealth.org.uk/publications
Scourfield, P. (2010). “Reflections of the serious case review of a female adult” (JK). Journal of Adult Protection, Vol 12, (4), 16-30.
Vygotsky, L.S. (1978). Mind in Society: The development of higher psychological processes. (M.Cole., V. John-Steiner, S. Scribner and E. Souberman, Eds). Cambridge, Massachusetts: Harvard University Press.
 Petition to NHS England - The Case for Funding Training in the NHS 2021
Alert!
Petition to NHS England - The Case for Funding Training in the NHS 2021
Alert!ACAT's online payment system has been updated - click for more information

Full Reference
Brown, H. and Lloyd, L., 2012. What is the 2005 Mental Capacity Act and how can CAT help us to make sense of the decision making process at its heart?. Reformulation, Summer, pp.35-42.Search the Bibliography
Type in your search terms. If you want to search for results that match ALL of your keywords you can list them with commas between them; e.g., "borderline,adolescent", which will bring back results that have BOTH keywords mentioned in the title or author data.
Related Articles
Confidentiality and Good Record Keeping in CAT Therapy - A Discussion Paper
Brown, H., 2010. Confidentiality and Good Record Keeping in CAT Therapy - A Discussion Paper. Reformulation, Summer, pp.10-12.
Consent to Publish in Reformulation
Jenaway, A., Lloyd, J., 2008. Consent to Publish in Reformulation. Reformulation, Summer, p.7.
Report from the Third CAT and LD Conference, in London
Baines, G., 2014. Report from the Third CAT and LD Conference, in London. Reformulation, Summer, pp.13-15.
The Awkward Silence - Ethics of Withholding Information
Oliver O’Mara, 2013. The Awkward Silence - Ethics of Withholding Information. Reformulation, Summer, p.9,10,11,12,13.
BOOK REVIEW: Cognitive Analytic Therapy for people with intellectual disabilities and their carers
Lloyd, J,. and Clayton, P., 2014. BOOK REVIEW: Cognitive Analytic Therapy for people with intellectual disabilities and their carers. Reformulation, Summer, pp.10-11.
Other Articles in the Same Issue
A Hopeful Sequential Diagrammatic Reformulation
Bradley, J., 2012. A Hopeful Sequential Diagrammatic Reformulation. Reformulation, Summer, pp.13-15.
Aims and Scope of Reformulation
Lloyd, J. and Pollard, R., 2012. Aims and Scope of Reformulation. Reformulation, Summer, pp.3-4.
CAT with People who Hear Distressing Voices
Perry, A., 2012. CAT with People who Hear Distressing Voices. Reformulation, Summer, pp.16-22.
Great Time: From Blade Runner to Bakhtin
Pollard, R., 2012. Great Time: From Blade Runner to Bakhtin. Reformulation, Summer, pp.32-34.
Letter from the Chair of ACAT
Hepple, J., 2012. Letter from the Chair of ACAT. Reformulation, Summer, p.6.
Letter from the Editors
Lloyd, J. and Pollard, R., 2012. Letter from the Editors. Reformulation, Summer, p.5.
Reflections on a Dilemma in a Supervision group: Caught between a Rock and a Hard Place
Gil-Rios, Dr. C., M., and Blunden, Dr. J., 2012. Reflections on a Dilemma in a Supervision group: Caught between a Rock and a Hard Place. Reformulation, Summer, pp.23-25.
Sleep Tight: Working Creatively with Dreams in CAT
Coulter, N. and Rushbrook, Dr S., 2012. Sleep Tight: Working Creatively with Dreams in CAT. Reformulation, Summer, pp.7-12.
The 16 + 1 interview
Petratou, V., 2012. The 16 + 1 interview. Reformulation, Summer, p.43.
Using a Cognitive Analytic Therapy approach in working with Eating Disorders: Reflections on Practice
Wicksteed, Dr. A., 2012. Using a Cognitive Analytic Therapy approach in working with Eating Disorders: Reflections on Practice. Reformulation, Summer, pp.26-31.
What is the 2005 Mental Capacity Act and how can CAT help us to make sense of the decision making process at its heart?
Brown, H. and Lloyd, L., 2012. What is the 2005 Mental Capacity Act and how can CAT help us to make sense of the decision making process at its heart?. Reformulation, Summer, pp.35-42.
Help
This site has recently been updated to be Mobile Friendly. We are working through the pages to check everything is working properly. If you spot a problem please email support@acat.me.uk and we'll look into it. Thank you.
