Generating Practice-Based Evidence for CAT
Marriott, M. and Kellett, S., 2007. Generating Practice-Based Evidence for CAT. Reformulation, Summer, pp.40-42.
Are we effective in routine adult mental health care? Should we be more cognitive when delivering CAT? The need for more practice based CAT evidence.
At the 2007 CAT conference we presented the findings from a service evaluation initiative that was commissioned to demonstrate the practice-based evidence of CAT with referrals in routine practice. Evidence for the psychotherapies has developed a cleavage between what are its evidence-based practice (EBP) foundations (the internally well-controlled randomised control trial of a therapy) and its practice-based evidence applications (PBE) (the ‘real world’ evaluation of effectiveness of a therapy, conducted in routine settings, which do not exclude clients for methodological reasons). For a therapy to attain empirical status and acceptance, it needs to have both EBP and PBE in equal and extant parts; to satisfy both the ‘scientist’ and the ‘practitioner.’
Data for the project was taken from an existing audit and evaluation system for clients referred to a psychological service from primary or secondary care. A sample of 65 clients who had received CAT were analysed for their assessment characteristics and clinical outcome, and this was compared with 180 clients who had received cognitive behaviour therapy (CBT) and 70 clients who had received person-centred therapy (PCT). Data was taken from two sources: (1) therapists (intervention length, presenting problem) and (2) clients (self-rated measures completed at the start and completion of therapy; the Beck Depression Inventory (BDI-II), The Inventory of Interpersonal Problems (IIP-32), and the Brief Symptom Inventory, BSI).
Contrary to assumptions that CAT clients are more likely to present with interpersonal difficulties or trauma, a significantly greater proportion of CAT clients were described as having depression as their main presenting problem, compared with those allocated to receive CBT or PCT, and only clients allocated to receive CAT were described as having a personality disorder or a psychotic disorder. The CAT sample was more distressed across all the assessment measures than clients in the other two services. A matched sample was then created of clients who had received either brief (6-16 sessions) or medium-term (17-30 sessions) interventions and who displayed similar levels of presenting psychopathology on the assessment global severity index (GSI) of the BSI. This was in order to compare like with like in terms of subsequent outcomes.
There was considerable variation in the number of sessions of CAT that clients received; with the majority of clients not receiving either of the usual intervention lengths suggested in CAT theory (16 or 24 sessions). Contrary to assumptions about allocation to a brief (up to 16 sessions) or medium-term (over 16 sessions) intervention, length of therapy could not be predicted based on assessment characteristics recorded in this study, as both the brief and medium term CAT groups appeared to be equivalently distressed. Further clarification within the CAT community appears necessary for elaborating on the process of allocation to shorter or longer interventions; explanations based on distress do not appear to be reflected in psychometric data.
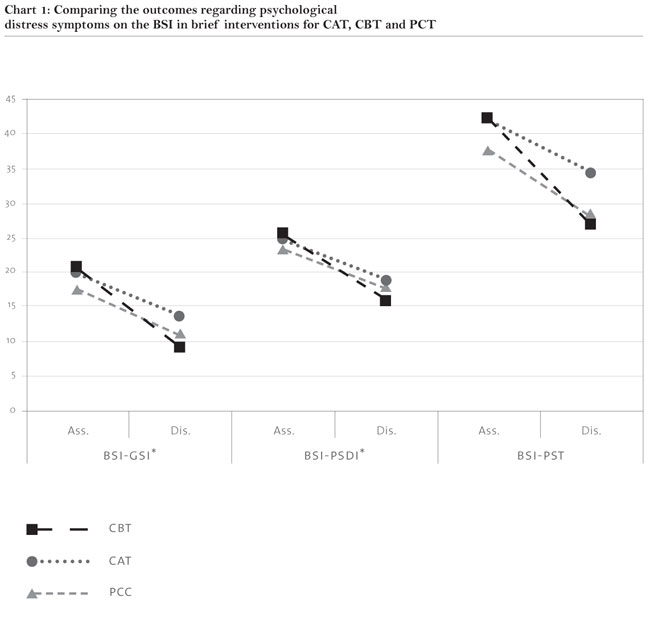
In terms of outcomes achieved, there was some suggestion that a longer CAT intervention improved outcome. This was seen in better mean improvement scores for the medium-term intervention, as well as more clients achieving a clinically reliable improvement. Whilst few of these differences were statistically significant, this comparative effectiveness of a longer intervention was clearer in the CAT service than the other two services. CAT appeared effective in terms of creating an improvement in psychological and interpersonal distress, and that it is comparable with other psychotherapies practised as standard in the NHS. There was a statistically significant trend however showing brief interventions of CBT to improve general psychological symptomatology at greater rates than does CAT, which is demonstrated in Chart 1. Within longer interventions, CBT and CAT were more similar across all measures used, and achieve slightly superior improvements in depression and interpersonal difficulties than PCT.
These outcome findings can raise questions about what CAT practitioners might wish to use as their default intervention length, suggesting that an alternative to the 16 session model might be worth considering. All of the findings should be approached with caution, due to the inherent methodological limitations of PBE. These included in the present evaluation:
- Unstandardised diagnostic labelling.
- Unstandardised interventions (e.g. practitioner length of experience, qualifications, level of supervision, and model consistency all unknown).
- Uncontrolled, non-random intervention allocation, and no qualitative data regarding participant allocation.
- Non-inclusion of clients who did not provide outcome data, and attrition rates unknown.
- Comparisons with just two other therapies.
- No control for whether individuals had presented just once or a number of times for therapy.
- No control for length of time on waiting list.
- No follow-up.
However, the findings do suggest questions that are worthy of further investigation or reflection amongst CAT practitioners. Particular questions of interest are whether CAT can or needs to be more symptom focussed and the means by which the CAT community can contribute to establishing a practicebased evidence base. Any services that would like a copy of the full report are invited to contact Steve Kellett for further information.
Michael Marriott
University of Sheffield, Clinical Psychology Unit, Dept. of Psychology, Western Bank, Sheffield, S10 2TP. email: pcp04mrm@shef.ac.uk
Stephen Kellett
Barnsley PCT NHS Trust, Psychological Health Care, 11/12 Keresforth Close, Barnsley, S70 6RS. email: stephen.kellet@barnsleypct.nhs.uk
References
Barkham, M. Hardy, G.E., & Startup, M. (1996). The IIP-32: A short version of the Inventory of Interpersonal Problems. British Journal of Clinical Psychology 35, 21-35.
Beck, A.T., Steer, R.A., & Brown, G.K. (1995). Beck Depression-II Manual. San Antonio, US: The Psychological Corporation, Harcourt Brace & Co.
Derogatis, L. R. (1993). Brief Symptom Inventory (BSI): Administration, scoring and procedures manual. (3rd Ed). National Computer Systems, Inc.
Comment by Tony Ryle
CAT therapists must not expect to win every contest on points. All three models reported were effective and the study does not entitle managers to appoint one rather than the other. Nor should we retire unthinkingly behind the many holes in the evidence presented. (e.g. the patients were allocated, it is not clear by what process or by whom, but the fact that PDs ended up with CAT may suggest a more general bias to send more severe cases that way). I think we should pause for thought. Maybe the variable length of CAT reflected not just the indiscipline of the therapists but judgement? It is very probable that more severe cases needing longer therapy. There might be a case for a flexible time frame, for example a 12-session contract to a review with a further number up to 24 negotiated; or maybe a decision based on psychometry with routine symptom scores indicating poor response leading to review and maybe extension. Maybe CBT works better for straightforward symptomatic disorders or maybe the CBT-like elements of CAT are not well done. e.g. TP and TPP monitoring and graphing, symptom diaries, exploring alternative behaviours and perhaps adding some specifics when indicated. Maybe CAT being problem focused should not rule out spending more time on solutions. Should there be some revisions to the training we provide?
In the words of Joe Hill, a great union man in the US in the 1920s, ‘Don’t mourn, organise!’ Anyone working in a service with both CBT and CAT therapists could design a totally ethical comparison, randomising cases with PSQ scores below 28, recording past history and drop-out rates, and following up or at least recording re-referrals.
 Petition to NHS England - The Case for Funding Training in the NHS 2021
Alert!
Petition to NHS England - The Case for Funding Training in the NHS 2021
Alert!ACAT's online payment system has been updated - click for more information

Full Reference
Marriott, M. and Kellett, S., 2007. Generating Practice-Based Evidence for CAT. Reformulation, Summer, pp.40-42.Search the Bibliography
Type in your search terms. If you want to search for results that match ALL of your keywords you can list them with commas between them; e.g., "borderline,adolescent", which will bring back results that have BOTH keywords mentioned in the title or author data.
Related Articles
The CAT Articles Review
Knight, A., 2009. The CAT Articles Review. Reformulation, Summer, p.32.
CAT Effectiveness: A Summary
Quraishi, M., 2009. CAT Effectiveness: A Summary. Reformulation, Summer, pp.36-38.
Evaluation of CAT in GP Practice
Baker, J., 2003. Evaluation of CAT in GP Practice. Reformulation, Spring, pp.16-17.
Measuring Outcomes in CAT
Freeman, E., Williams, L., 2008. Measuring Outcomes in CAT. Reformulation, Winter, p.14.
Clinical Outcomes Of Cognitive Analytic Therapy Delivered By Trainees
Darongkamas, J., Newell, A. Hewitt-Moran, T. & Jordan, S, 2017. Clinical Outcomes Of Cognitive Analytic Therapy Delivered By Trainees. Reformulation, Winter, pp.38-42.
Other Articles in the Same Issue
Book Review: Just War. Psychology and Terrorism
Collins, S., 2007. Book Review: Just War. Psychology and Terrorism. Reformulation, Summer, pp.18-19.
Case Study on Z not as Impossible as we had Thought
Lloyd, J., 2007. Case Study on Z not as Impossible as we had Thought. Reformulation, Summer, pp.31-39.
Generating Practice-Based Evidence for CAT
Marriott, M. and Kellett, S., 2007. Generating Practice-Based Evidence for CAT. Reformulation, Summer, pp.40-42.
Keeping cat alive
Ryle, A., 2007. Keeping cat alive. Reformulation, Summer, pp.4-5.
Reformulating the NHS reforms
Jones, A. and Childs, D., 2007. Reformulating the NHS reforms. Reformulation, Summer, pp.7-10.
The Application of CAT to Working with People with Learning Disabilities
Moss, A., 2007. The Application of CAT to Working with People with Learning Disabilities. Reformulation, Summer, pp.20-27.
The Inner Voice Check
Elia, I., 2007. The Inner Voice Check. Reformulation, Summer, pp.28-29.
Using CAT in an assertive outreach team: a reflection on current issues
Falchi, V., 2007. Using CAT in an assertive outreach team: a reflection on current issues. Reformulation, Summer, pp.11-17.
You’re driving me insane: Literature, Lyrics and Drama through CAT eyes for clients and students
Elia, I. and Jenaway, A., 2007. You’re driving me insane: Literature, Lyrics and Drama through CAT eyes for clients and students. Reformulation, Summer, pp.43-44.
Help
This site has recently been updated to be Mobile Friendly. We are working through the pages to check everything is working properly. If you spot a problem please email support@acat.me.uk and we'll look into it. Thank you.
