How CAT-Informed Practice Can Help To Improve Mental Health Services
Ben Bell, 2017. How CAT-Informed Practice Can Help To Improve Mental Health Services. Reformulation, Winter, pp.33-37.
Introduction
Since training as a CAT therapist, I have learnt a lot about both myself and the mental health system I work in as a case manager in an Early Intervention Team (‘case manager’ or ‘care coordinator’ are blanket terms used for qualified social workers, mental health nurses or occupational therapists working in NHS mental health teams). I believe that this learning, based on CAT principles, has the potential to improve the service we provide as mental health professionals, and that CAT can be used in an integrative way across all roles - psychiatry, psychology, case management, assistant practitioner and peer support worker roles.
I have used CAT informed practice in my team where I have worked with a CAT qualified psychologist. This helpful way of working, and a number of thoughts that arise on reflection, are described in the article below. For point of reference, I also refer the reader to previous articles in Reformulation that have discussed CAT skills training in mental health settings, such as that by De Normanville and Kerr (2003) which specialises in personality disorders and is accredited by ACAT as a skills level training, as well as an article written by Annesley and Jones (2016) on ‘The 4P’s model: A CAT derived tool to assist individuals and staff groups in their everyday clinical practice with people with complex presentations’.
Such training and models have gained positive feedback from the clinical teams that have and continue to implement them, such as an improved understanding of and communication with clients, better preventative work, and more value placed on reflective and relational learning and practice (Freshwater and Kerr, 2006; Annesley and Jones, 2016).
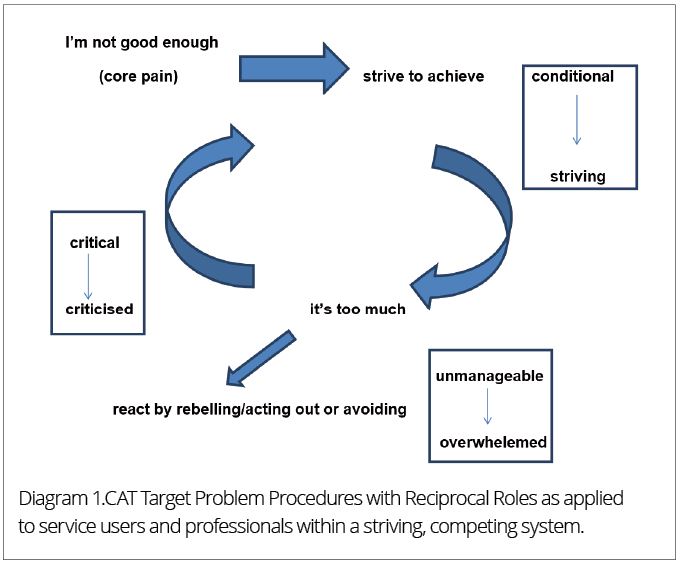
For the purposes of this article, I will discuss how a CAT informed service can work to better help service users, and at the same time can provide us, as clinicians, with a greater awareness of the often problematic roles that we ‘play out’ as professionals. I begin by describing how Ryle and Kerr’s CAT-based model of psychotic disorder (2002) differs from the medical model, as this model applies specifically to service users in the Early Intervention team I work in, but it can be taken more generally to encompass all areas of mental health (for specific ways in which CAT is used in different areas of mental health, please refer to Ryle and Kerr (2002)).
The article will also involve a critique of healthcare systems as hierarchical, statistical and evidence-based environments and proposes that the concomitant striving to attain targets required of those working in these contexts can and, I believe, does work to undermine CAT principles and the benefits that these can bring to clients, clinicians and the organisation.
How the medical model and CAT based model of psychotic disorder differ
Ryle and Kerr’s CAT model of psychotic disorder looks at symptomatic psychotic states, such as auditory hallucinations, ‘voices’, and paranoid delusions, in terms of their interpersonal origins and the internalised reciprocal role procedures (RRPs) that are enacted, such as self-critical or self-sabotaging ways of relating. This approach encourages the service user and the clinician to form ‘a joint, meaningful, narrative of their story and experiences’ (2002: 166).
This approach can seem very different to a more medical-model approach to mental health care. In the team I work in, for example, the service user is assessed in order to determine symptoms, diagnosis and treatment. Psychiatrists are trained in determining these outcomes, and prescribing medication, whilst the case manager allocated to the service user attempts to form a more regular therapeutic relationship with them. However, as I have stated in the introduction, a CAT approach has the potential to work across all roles and disciplines, to add to and enhance clinicians’ previous training.
Where a familiar feature of the mental health profession is a lack of resources and often unmanageable caseloads, such a therapeutic relationship between clinician and service user can be limited. In such instances, medication could be seen as the primary route for processing persons with psychological difficulties, in the sense that its supply and demand is not affected by the above lack of resources. But regardless of lack, the medical model has been extensively criticised and a need identified for a wider and more in-depth understanding of service users’ social, biological and psychological experience beyond their diagnosis (Kinderman and Cooke, 2000).
A medical service framework does not however inhibit health services from making use of a CAT-informed way of working, or culture, to potentially gain a more in-depth and meaningful understanding for both service users’ and professionals’ experiences, despite the above-mentioned drawbacks.
CAT-Informed Work
Where there are limitations in providing a more in-depth understanding of service users’ experience, due to a lack of resources and the medical model, CAT can provide a common language and set of understandable tools to aid the clinician’s and service user’s relationship. During the course of a CAT therapy, one of the aims of the therapist is to be explicit with the client early on about what is realistic in terms of what can be achieved together in the therapy. This introduces the idea of limitations, which is a crucial part of the CAT therapeutic process in aiding the client to address the realistic as opposed to the idealistic, perfectionist or fantasy views of the world that they may hold, which of course are unsustainable.
So it follows that in CAT-informed work with service users, for the clinician to be honest and transparent about the limitations of their service and what it can offer is an important step in building a realistic, as opposed to a false or disingenuous, therapeutic relationship. But of course, people – service user and professional alike – can struggle with limitations. From a CAT point of view, these can be related to our early-life experience, where needs were not met by a caregiver, and so as adults we can still unconsciously want these needs to be met.
It should be noted here that despite the positive level of honesty and transparency mentioned above, professionals need to use discretion where different service users are at different levels of development – to use CAT terminology, their zone of proximal development (ZPD). Therefore, to be too explicit with certain service users about a service’s limitations could be un-containing and negatively affect them in terms of the trust they have in it, as well as in you as a clinician.
People can suffer from mental health conditions where their feelings have not been allowed to be expressed and understood in a safe way. Thoughts and feelings can then become internalised, or acted out in confused or dangerous ways, such as self-harm, conflicts with or avoidance of others. As adults, we can re-play the strategies we decided upon as infants in order to survive or cope. The reason we do this is because psychologically we are still hoping to resolve the basic issue that was left unresolved in infancy – how to obtain unconditional love and the relational conditions that enable optimal infant, child and adult development.
Confronted with the limitations of a mental health service, or any service provision, the need to be ‘fixed’ or cured, can become easily frustrated, because the need may be unmet, as well as unrealistic. CAT was designed to be used within such a system, in terms of offering a shorter term therapy to overcome the excesses of other longer term therapies. If needs are not met, unrealistic or otherwise, then the relationship between mental health professionals and service users can become problematic in numerous ways, and present barriers to this relationship. I worked with the psychologist in our team to present CAT-informed work, including a case study and diagrams, to show how such barriers can occur.
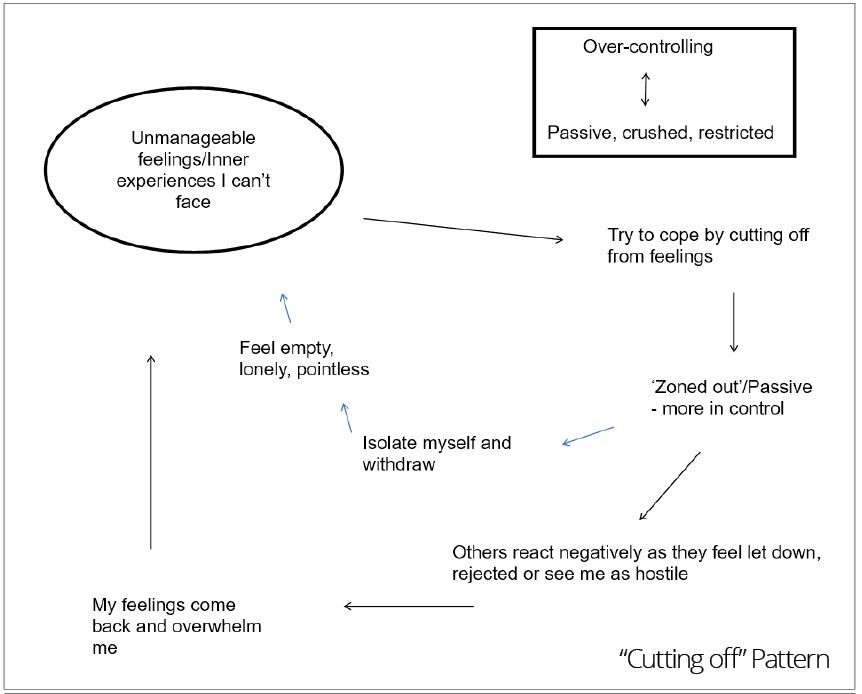
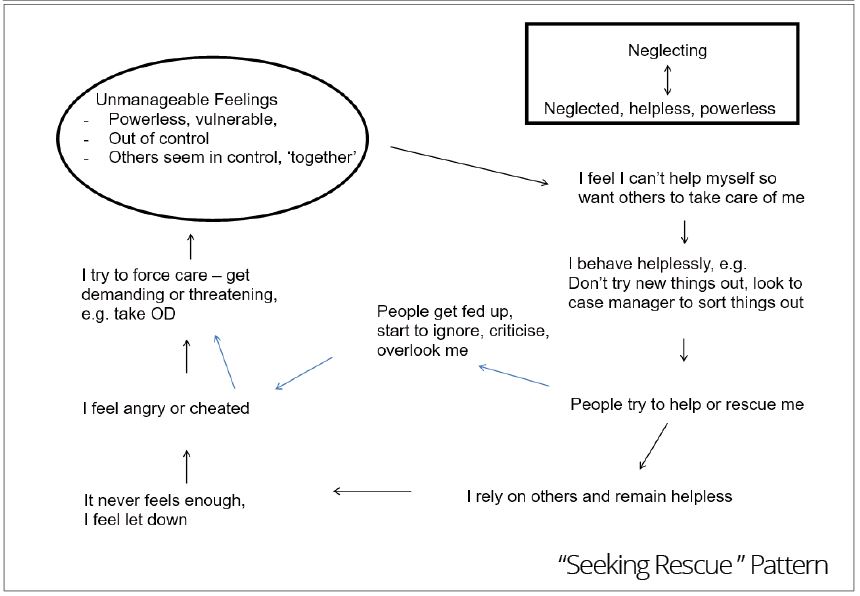
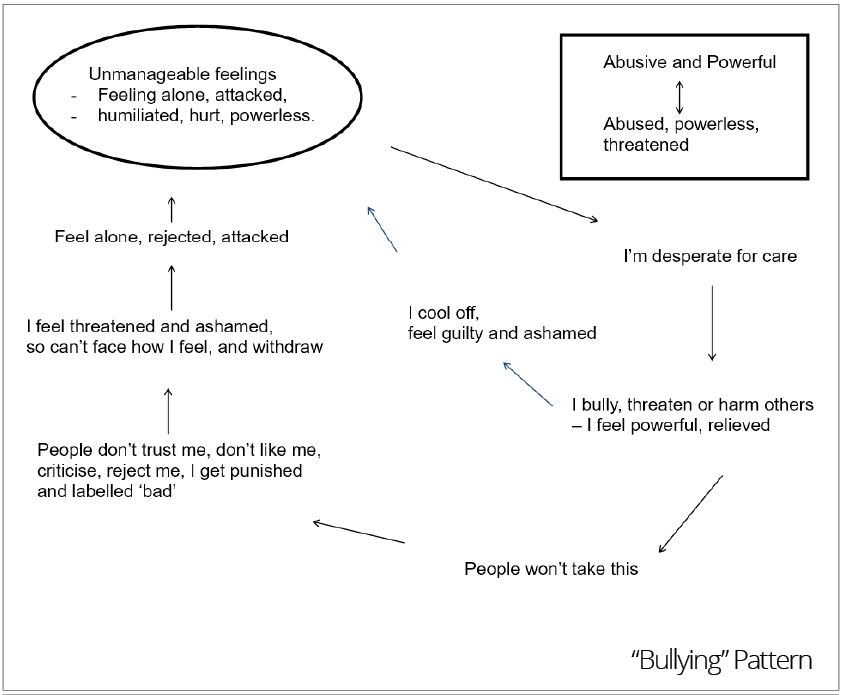
We used three diagrams to chart out the patterns or target problem procedures (TPPs) that service users can enact with us and others, using three self-states: cutting off, seeking rescue and bullying (see Appendix 1). As you can see in the diagrams, the reciprocal roles (RRs) we labelled were: controlling-to-passive or crushed (cutting off), neglecting-to-neglected (seeking rescue), and abusive and powerful-to-abused, powerless or threatened (bullying).
Where service users enact a cutting off procedure, I can feel that I need to try harder, where their response to my intervention is to become passive or withdraw. A transference (referred to in CAT terminology as ‘the dance’ or enactment) can also occur, where the service user’s feelings of pointlessness can be ‘projected’ onto me, and I can then feel that my interventions are pointless, and become despondent, in turn feeling defeated or dismissed. With the external demands of the system I work in – meeting targets, increasing caseloads and so on – also feeling over-controlling, I can then, like the service user met with controlling circumstances of their own, choose to zone out and isolate myself.
In CAT-informed work, to try and name the feelings that are not given a voice here between myself and the service user is necessary to build a more purposeful and productive therapeutic relationship. From the cutting-off position on the diagram, one of the unexpressed or unmanageable emotions the service user experiences is loneliness. For someone that enacts a cutting-off state, any discussion or naming of such emotions will likely be very difficult, and there are no hard-and-fast rules for how to approach this, but for me to realise what is going on for them from a CAT perspective, means that I can try to avoid the transference, or dance, that their behaviours might elicit in me. This in turn has the potential to model a different relationship for the service user than those they are used to, where talking about ways of relating, emotions and behaviours are not discussed, which prevents their TPPs from changing.
Likewise, with a service user that seeks to be rescued, I can reciprocate and become ‘the rescuer’, reinforcing their helpless role, which does not empower them, but will likely cause me to become frustrated and resentful of their over-reliance on me, not to mention my feeling exhausted. I could also feel that I have failed when the service user becomes disappointed and unsatisfied that the ideal caring role they are unrealistically seeking cannot be sustained. If, however, I am able to create a dialogue around the subject of the service user’s natural sense of disappointment when the fantasy or compensatory elements of their map proves inconsistent with reality, then a more authentic relationship has a chance to develop.
Finally, with the bullying state in mind, the behaviours of service users that can be critical, rejecting or threatening of services can be reciprocated - mirrored back to them unconsciously where professionals can react in similar, if understandable, rejecting ways. To talk with the service user about the underlying and difficult or unbearable feelings that underlie and maintain their rejecting behaviour, such as vulnerability, loneliness and powerlessness, can lead to understanding and a way to find exits, such as changes to their ways of relating and thereby avoidance of future rejecting or similarly negative enactments.
Using CAT methods to talk about service users and how we relate to them in team meetings is another way of introducing CAT-informed work to our practice and is a further way that my team have utilised reflective practice in the workplace. The psychoanalyst Isabel Menzies-Lyth (1988), best known for her work on unconscious processes in institutions, has written about defence mechanisms becoming institutionalised where reflective practice and relationships are not encouraged, and how such defences can intensify through increased risk and the anxious reactions it provokes (Joffe, 1999). From the three examples of self-states above, it is easy to see how such defence patterns and anxious reactions can increase.
Alongside the three diagrams described, our presentation to our clinical team included another diagram (see diagram 1 below) to describe how both clinician and service user alike can enact roles within the type of demanding system I have described.
Conclusion
In this paper I have discussed how the use of CAT can bring us as clinicians and as service users into greater awareness of how we are affected negatively by the limitations of our present system. This system, both hierarchical and dominantly medicalised, has been criticised for its limited way of viewing individuals, their problems and how to ‘treat’ them. One suggestion of how to affect change at a team-level is for CAT trainees or practitioners to educate their teams in CAT-informed work, so that all staff can be trained in therapeutic skills and concepts to create a common language through which relational understanding can develop to inform and maintain change for the service user, clinicians and the organization.
References
De Normanville, J. and Kerr, I.B. (2003) Initial experiences of a CAT skills level training in a CMHT. Reformulation, 18; 25-27 (Available through www.acat.me.uk).
Freshwater, K. and Kerr, I. (2006) CAT Skills Training in Mental Health Settings, Reformulation, Summer pp. 17-18. (Available through www.acat.me.uk).
Joffe, H. (1999) Risk and ‘the other’, Cambridge: Cambridge University Press.
Kinderman, P. and Cooke, A. (2000) Recent advances in understanding mental illness and psychotic experiences: A report by the British Psychological Society Division of Clinical Psychology, The British Psychological Society.
Menzies-Lyth, I. (1988) Containing Anxiety in Institutions: Selected Essays, Volume 1, London: Free Association Books Ltd.
Phyllis, A. and Lindsay, J. (2016) The 4P’s model: A Cognitive Analytic Therapy (CAT) derived tool to assist individuals and staff groups in their everyday clinical practice with people with complex presentations. Reformulation, Summer pp.40-43 (Available through www.acat.me.uk).
Ryle, A. and Kerr, I. B. (2002) Introducing Cognitive Analytic Therapy: Principles and Practice, Chichester: Wiley.

Full Reference
Ben Bell, 2017. How CAT-Informed Practice Can Help To Improve Mental Health Services. Reformulation, Winter, pp.33-37.Search the Bibliography
Type in your search terms. If you want to search for results that match ALL of your keywords you can list them with commas between them; e.g., "borderline,adolescent", which will bring back results that have BOTH keywords mentioned in the title or author data.
Related Articles
Helping service users understand and manage the risk: Are we part of the problem?
Crowther, S., 2014. Helping service users understand and manage the risk: Are we part of the problem?. Reformulation, Winter, pp.41-44.
The 4P’s model: A Cognitive Analytic Therapy (CAT) derived tool to assist individuals and staff groups in their everyday clinical practice with people with complex presentations
Phyllis Annesley and Lindsay Jones, 2016. The 4P’s model: A Cognitive Analytic Therapy (CAT) derived tool to assist individuals and staff groups in their everyday clinical practice with people with complex presentations. Reformulation, Summer, pp.40-43.
The Idealised Care Smokescreen: How the Tools we Share can be Used to Attack
Julia Coleby and Kate Freshwater, 2019. The Idealised Care Smokescreen: How the Tools we Share can be Used to Attack. Reformulation, Summer, pp.13-16.
'Five Session CAT' Consultancy: Using CAT to Guide Care Planning with People Diagnosed within Community Mental Health Teams: Brief Summary Report
Dr Angela Caradice, 2013. 'Five Session CAT' Consultancy: Using CAT to Guide Care Planning with People Diagnosed within Community Mental Health Teams: Brief Summary Report. Reformulation, Winter, p.15,16,17,18,19.
“We need decent people as well as decent lawsâ€:
Beth Greenhill, Amanda Roberts and Rebecca Swarbrick, 2013. “We need decent people as well as decent lawsâ€:. Reformulation, Summer, p.18,19,20,21,22,23,24,25.
Other Articles in the Same Issue
A case study of cognitive analytic therapy with a client diagnosed with psychotic depression
John Cartmell, 2017. A case study of cognitive analytic therapy with a client diagnosed with psychotic depression. Reformulation, Winter, pp.22-27.
An Alternative Psychotherapy File
Alison Jenaway, 2017. An Alternative Psychotherapy File. Reformulation, Winter, p.48.
Austerity, Power and CAT’s Opportunity for Change
John Cartmell, 2017. Austerity, Power and CAT’s Opportunity for Change. Reformulation, Winter, pp.5-7.
Clinical Outcomes Of Cognitive Analytic Therapy Delivered By Trainees
Darongkamas, J., Newell, A. Hewitt-Moran, T. & Jordan, S, 2017. Clinical Outcomes Of Cognitive Analytic Therapy Delivered By Trainees. Reformulation, Winter, pp.38-42.
Concepts of the Self, Social Inequality, Culture and Power in reflecting on therapeutic work with Asylum Seekers and Refugees: A Cognitive Analytic Approach
Dr Claire Wilson, 2017. Concepts of the Self, Social Inequality, Culture and Power in reflecting on therapeutic work with Asylum Seekers and Refugees: A Cognitive Analytic Approach. Reformulation, Winter, pp.44-47.
How CAT-Informed Practice Can Help To Improve Mental Health Services
Ben Bell, 2017. How CAT-Informed Practice Can Help To Improve Mental Health Services. Reformulation, Winter, pp.33-37.
On Learning From Our Patients: Reformulating CAT Training
Robert Marx, Joanne King, Kylie, Mary Wilson-Verrall, Karen Spencer and Annabel J McDonald, 2017. On Learning From Our Patients: Reformulating CAT Training. Reformulation, Winter, pp.13-18.
Perfectly Imperfect: Reflections of a Newly Qualified Clinical Psychologist in using CAT to Explore the Relational Contribution to Binge Eating
Dr Lyndsey Holt, 2017. Perfectly Imperfect: Reflections of a Newly Qualified Clinical Psychologist in using CAT to Explore the Relational Contribution to Binge Eating. Reformulation, Winter, pp.28-32.
The Clinician’s Guide To Forensic Music Therapy - Book Review
Wakeling, N, 2017. The Clinician’s Guide To Forensic Music Therapy - Book Review. Reformulation, Winter, pp.56-57.
Using The Parent-Adult-Child Model Alongside CAT
Louise Elwell, 2017. Using The Parent-Adult-Child Model Alongside CAT. Reformulation, Winter, p.43.
When Therapy Feels Like A Roller Coaster Ride: A CAT Perspective
Dr Diane Agoro, 2017. When Therapy Feels Like A Roller Coaster Ride: A CAT Perspective. Reformulation, Winter, pp.19-21.
Where Should We Keep Reformulation Letters?
Kate Freshwater, Tilait Tanweer & Wendy Walker, 2017. Where Should We Keep Reformulation Letters?. Reformulation, Winter, pp.8-12.
Help
This site has recently been updated to be Mobile Friendly. We are working through the pages to check everything is working properly. If you spot a problem please email support@acat.me.uk and we'll look into it. Thank you.