Creatively Adapting CAT: Two Case Studies from a Community Learning Disability Team
Smith, H., Wills, S., 2010. Creatively Adapting CAT: Two Case Studies from a Community Learning Disability Team. Reformulation, Winter, pp.35-40.
Introduction
Historically, people with learning disabilities have been excluded from psychotherapies due to their degree of intellectual impairment, with treatments being almost exclusively behavioural in their approach (Bender, 1993). Valerie Sinason criticised the view that people with learning disabilities would not benefit from psychotherapy. She differentiated between cognitive and emotional intelligence, proposing that the two are not necessarily linked. Indeed, she described how it could be possible for an individual’s emotional intelligence to develop age appropriately, whilst having severe deficits in cognitive intelligence (Sinason, 1992). Thus we should not assume that individuals with intellectual impairment do not have the capabilities to engage effectively in psychotherapy (Department of Health, 2001).
There is now a growing array of literature describing how some psychotherapies have been adapted for use with people with learning disabilities. Brown and Marshall (2006), for example, adapted Cognitive Behavioural Therapy for a woman with mild learning disabilities.
The NHS is currently exploring ways of increasing access to psychological therapies (IAPT) to all client groups. As part of this, our NHS Community Learning Disability team has begun to look at adapting Cognitive Analytic Therapy (CAT) for individuals with a learning disability. With its inherently creative qualities, CAT lends its hand well to this client group; indeed, with modification, the tools of CAT can be successfully used (Ryle and Kerr, 2002).
In this paper, we will discuss how we have used CAT to provide psychotherapy for two individuals with a learning disability, whilst considering the following:
- What do you need to take into account when working with people with learning disabilities?
- What is different when working with people with learning disabilities in comparison to other client groups?
- Does the presence of a learning disability prevent an individual from actively engaging in CAT?
The Authors
We both joined Sussex Partnership NHS Foundation Trust at the beginning of 2008 as assistant psychologists within the community learning disability team; shortly after this we took an interest in exploring ways of adapting CAT for adults with a learning disability. We attended a newly set up CAT supervision group run by Hilary Brown, where we could share ideas and experiences, discuss how we were adapting some of the CAT tools and reflect on this learning process, enabling us to progress with our CAT focused client work.
Case Example 1 – Donna
On moving to a new area, into a recently opened residential service in a community setting, Donna’s G.P. was prompted to make a referral to the Community Learning Disability Team on account of her complex history. A summary psychiatric report accompanied the referral and detailed seriously risky behaviours, including walking along a motorway and jumping in front of cars.
Donna, a 48 year old woman, was the youngest of six children, having four older brothers and one older sister. As a child, Donna initially attended a mainstream school for six months, but soon after she was moved to a school for children with learning disabilities. Her parents separated early in her childhood. She did not know her father well and lost contact with him from an early age. She was brought up by her mother and they were close. Donna was admitted to hospital under the Mental Health Act at the age of 20, where she spent two years. There then followed various similar admissions and many recorded incidents of absconding and threats of suicide. At the age of 47, Donna moved to her current residence, a residential service for adults with learning disabilities. The house was staffed with support workers 24 hours a day.
Donna had a moderate learning disability. She did not read, but could copy letters and spell words with sufficient levels of support.
Donna and I (SW) met for a total of 24 sessions over 8 months, with one follow-up session after a break of 6 weeks.
Case Example 2 – Julie
Julie was referred to the Community Learning Disability Team by her home manager for counselling. In Julie’s review, prior to her referral, it was suggested that she might benefit from having some counselling sessions, whereby she could develop ‘control techniques’ to use when she threw ‘wobblies’. The home manager also explained how they hoped counselling would ‘lessen her challenging behaviours’.
Julie, a 34 year old woman with a moderate learning disability, was an only child and grew up living with her parents. Julie appeared to have a very supportive family and would regularly spend time with her parents, relatives and friends from home. Historically, Julie found it hard to engage with health professionals. A review of her case notes revealed several occasions when Julie had ‘absconded’ prior to scheduled appointments with professionals. In addition, she has often refused to see professionals for one-to-one support and counselling.
When Julie was 19 she moved to a residential service for adults with learning disabilities and has continued to live in this home with six other residents. The home provides 24 hour residential care.
Julie communicates verbally; however, input from speech and language therapy indicated that, despite her confident presentation when socialising and communicating, she may not always fully understand what people are saying. Julie and I (HS) met for a total of 24 sessions over a period of 6 months, with 2 follow-up sessions.
Trust and the Therapeutic Relationship
Donna
Donna found it hard to trust people. She spoke of having bad experiences of doctors not believing her in the past, and this was reflected in her ending every sentence with “I’m not lying”. Because she felt heavily dependent on staff to speak for her, the prospect of having to do this herself was perhaps too overwhelming and frightening for her, hence her insistence on having care staff present in the sessions with her. Initially, however, this was not a hindrance, as it made her reciprocal roles more apparent as they were acted out in sessions.
Neglected – Neglecting
When staff shortages made it difficult for staff to attend the sessions with Donna, I saw her acting out the ‘neglected’ pole. When Donna showed her reluctance to come into sessions, I saw her acting out the ‘neglecting’ pole. So it was as if she was neglecting me before I could neglect her, as it seems she was imagining I would do. For the first 12 sessions, Donna was reluctant to meet with me and I was continually confronted with “I don’t want to see her today” or “it’s a waste of time” or “I’m too busy today” etc. During one session, Donna was physically avoiding me. She replied that she did not want to see me today. I told her that I would wait in the visitor’s room for her until our session was scheduled to finish, to which she told me that I could wait all day if I liked but she still would not be attending the session. However, when Donna saw that I had brought more pictures with me, she joined me. I showed her a diagram representing the pattern of behaviour she presented at the beginning of every session (Diagram 1). I showed Donna how each week she didn’t want to see me and would fold her arms, but by the end of each session she was happily talking to me.
Diagram 1: Pattern of behaviour in therapy sessions
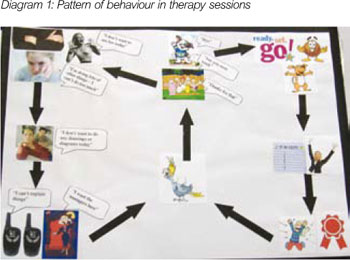
I suggested that perhaps next week she could follow the alternative cycle and be ready and willing to begin our session. Interestingly, the following week, she was again reluctant; however, she began engaging well shortly afterwards. In the sessions that followed, Donna began answering the front door and welcoming me into the house.
Julie
Initially Julie found it quite difficult to trust me and struggled to engage with the sessions. During the course of the therapy sessions, Julie experienced a high staff turnover in her home and as a consequence she appeared to find it difficult to trust the care staff and professionals including me. When reviewing Julie’s case notes, it was clear that this was not a new experience for her. In the past she had repeatedly found it difficult to work with health professionals and care staff and would often run away when appointments were scheduled.
Rejected – Rejecting
At this point, I hypothesised that Julie was all too familiar with people coming in and out of her life and when people did stay with her she had lost faith in developing a stable relationship with them. As a result I thought she was likely to sabotage the opportunities to develop meaningful and safe relationships by rejecting people before they rejected her – a common reciprocal role identified by Psaila and Crowley (2006).
To explore this, when Julie rejected me, I stayed with her. I waited for Julie downstairs and let her know every 15 minutes that I would stay there until she was ready to join me. In the following session I stayed in the room with Julie, but in silence. In this session she did not want to talk but she wanted me to stay with her. It took a few sessions for Julie to learn to trust me but by staying with her we were able to challenge her belief that people would always so easily reject or neglect her.
Julie found the goodbye letter very difficult to accept. She engaged well after we had named and challenged her beliefs about people leaving, yet would frequently divert my attention to other subjects whenever I tried to introduce my goodbye letter in the ending sessions. She would often ‘over talk’ when I brought the letter into the sessions. I predicted that she would find it difficult for this relationship to end. Prior to reading the goodbye letter, I named how I thought she was talking over me to cover this pain. With this recognition she allowed me to read the letter; however she refused to discuss it in any great detail.
Lack of Independence
Donna
It had been agreed at an initial assessment meeting that therapy sessions would take place at the residential service in which Donna lived, due to her dependence on staff to transport her to sessions and concerns that staff shortages may result in sessions being cancelled. This did, however, have consequences for building a therapeutic relationship. Staff would often sit in on our sessions during the early stages and this seemed to make Donna feel even more reliant on them for help with her communication, to the extent where she would only talk to me through the staff.
Controlled – Controlling
In terms of reciprocal roles, on the one hand, Donna wanted to be independent. She wanted to move out and live independently, she wanted to make new friendships outside of the home and she wanted to go out by herself. However, on the other hand, she wanted help from staff and came across as being extremely reliant on them to talk for her out of a fear of looking stupid or getting it wrong. Furthermore, Donna carried a two-way radio throughout the sessions so that she could contact staff when she wanted.
Donna switched so that sometimes people would talk for her and she’d feel controlled and other times she’d be controlling and bossy toward others. Donna was not aware of this reciprocal role. By naming it, acting it out in role play and representing it with pictures, Donna was able to recognise these roles. For example, when Donna picked up her two-way radio to shout instructions at staff, she laughed in response to my naming her ‘controlling’ role, commenting: “Oh yeah, I shout, tell staff what job to do”. At the same time, she waved her finger at me as if telling me off. I then held up a picture to Donna of two business women, who had a likeness to the home managers, to represent her ‘controlled’ role, she remarked: “they’re the managers – tell me what to do”.
Julie
Sometimes the care staff were very supportive of the therapy sessions by helping Julie to maintain helpful patterns of behaviour. However, I think that for some people with a learning disability this may not always be the case because of their level of dependence upon staff to support them in activities. Indeed, it is not uncommon for residential services to experience staff shortages, making it difficult for clients to get the one-to-one support they require to help them practise the ‘exits’ they develop during their therapy sessions.
Another example of how Julie depended on the staff was when they supported her to travel to the Community Learning Disability Team (CLDT) base for her sessions. Initially, I went to Julie’s home as it was difficult to make arrangements with Julie and the staff to travel to the CLDT base. However, by highlighting to the staff that she had the opportunity and right to have therapy sessions in the community, like other client groups receiving therapy, they arranged to support her to travel to the CLDT. This helped Julie to feel more in control of her appointments and it reinforced the value of her therapy to the care staff.
Confidentiality and Working with Care Staff
Donna
Donna had no experience of this type of one-to-one psychotherapy before, and little understanding of confidentiality, having always thought that care staff and family need to know everything that she does and feels.
Because of Donna’s insistence on having care staff in the sessions with her, allowing her to experience confidentiality was difficult. As the sessions progressed and our trust developed, Donna would reluctantly agree to come into the sessions on her own. Confidentiality was still a challenge, since, at the end of each session, she would instruct me to tell staff what we had spoken about during our session, saying that she could not remember.
As we started to use pictures and diagrams to talk in order to explore Donna’s thoughts and feelings, she would still rush out at the end of each session as she wanted staff to know what we had spoken about, but this time she could show them her work instead of instructing me to tell staff. As highlighted by Bancroft et al (2008), issues of confidentiality require careful consideration and, whilst by sharing her diagram with care staff Donna gained some independence and a voice, it may be equally important to address her right to confidentiality.
Julie
My work with Julie incorporated the use of lots of different communication methods and tools, such as talking, drawing and writing, to name a few. At the beginning we discussed in detail the confidentiality issues and boundaries that we would adhere to. Despite Julie’s wish to keep the issues that arose in the sessions private, she would often show the work we did together to the staff in her home. When she did this it seemed as if she wanted to please the staff and show them that she was ‘good today’. These instances showed me how Julie felt she was viewed by staff and how she was expected to ‘be good’. When finishing one session, I was met by a support worker who asked whether Julie had been good. At this point her head lowered and she withdrew from the conversation. I think that it was a challenge for me as Julie’s therapist, and for Julie to keep communicating the confidentiality issues to the staff team. I can imagine that this may be a similar experience for other people with learning disabilities, in that the staff are not always aware of the privacy issues within therapy. I believe it is important that the confidentiality is highlighted to the staff team as well as the client, in order to provide reassurance that the issues discussed in therapy are contained within the therapeutic space.
Towards the end of Julie’s course of therapy there were considerable staff changes. The service quality improved and Julie was able to begin developing positive relationships with the new members of staff. This helped when she was using her ‘exits’ identified in the therapy (Diagram 2).
Diagram 2: Exits
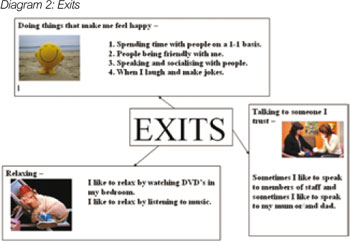
Julie requested that this part of her therapy was shared with the staff team and she asked for their help in applying these exits to her life. This support became really effective for the therapy and helped her to maintain more helpful patterns of behaviour.
Cognitive Ability
Donna
Initially, Donna was reluctant to speak for herself and requested staff to explain things for her, complaining that she could not explain things very well herself. This was perhaps an expression of what Sinason referred to as a ‘secondary handicap’, whereby it was better for Donna to pretend she was unable to recount experiences than for it to be proved to her that she could not recount experiences (Sinason, 1992).
On asking Donna a question, there would be either no response or a reply of “the manager can explain that to you”. Donna had the tendency to hear what she thought you would say, interpreting everything in a negative light. Past experience may have been justification for this way of thinking, when remarks such as, “they might think I’m stupid and lock me away”, are taken into consideration. It was almost as if there was a fear of being found out, and a fear of not being able to do something.
In the early stages of our meeting for sessions, we explored many ways of communicating (for example, writing a diary and summary sheets), none of which worked because of the dependence upon staff to help. As we discovered more concrete ways of communicating such as using pictures, Donna’s confidence grew, and she became more independent in her communication.
Julie
Julie struggled to recall her childhood experiences in great detail. The story she told me about her life seemed very fragmented and she appeared distressed when trying to recall parts. However, despite Julie’s difficulty in recalling events, I learnt what it was like to forget past experiences. As part of the therapy, we looked at photos of the people in her life and created a ‘people tree’. We called it a ‘people tree’ rather than a family tree as there were not many family members in her everyday life, but instead lots of care staff. By doing this collaboratively, she was able to tell me what people meant to her and we were able to establish some of her experiences with these people.
Some of the concepts used in CAT were difficult for Julie to understand. At times I would rephrase the language to assist her understanding. For example, when referring to reciprocal roles, instead of simply naming them, I described them by referring to everyday situations. She understood where these roles were in her life and also in other people’s lives; however, she found it difficult to understand the more abstract concept behind it. This adaptation to my approach did not seem to create difficult boundaries to our work but encouraged me to be more creative when working with her.
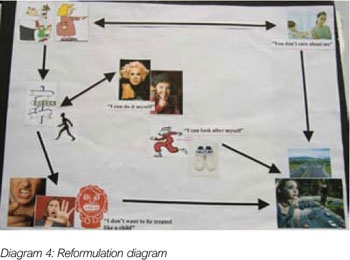
Furthermore, Julie struggled to read long prose. Therefore, instead of presenting the reformulation in the form of a letter, I presented it to her in a diagram (Diagram 3). By doing this she was able to understand her target problem procedure and refer to it in therapy and independently outside of the sessions.
Diagram 3: Reformulation diagram

Creative Communication
Donna
For the first 6 sessions, many different approaches to communicating were tried, but it was clear that talking alone, writing, reading, or remembering, were not helpful for Donna. I therefore decided to create a reformulation diagram (Diagram 4) with Donna with the aim of forming a collaborative relationship.
Diagram 4: Reformulation diagram
The pictures for the reformulation diagram had been sourced and prepared in advance; they were laminated and had Velcro on the reverse side. We used an ordinary door mat upon which to attach the pictures and arrows.
When Donna feels controlled, she can either conform or rebel. If she conforms and follows the rules, she gets angry and bossy, which leads to eliciting care through alarming means such as threats of suicide and walking along motorways. If Donna rebels, she runs away and again elicits care. When Donna feels neglected and ignored, she again seeks to elicit care. This perhaps shares similarities with the ‘rebel role’ described by Fisher and Harding (2009). When Donna rebelled in reaction to the notion of controlling care, this control increased, putting further restrictions on her independence, thus making her more angry, and so the cycle continued.
As I began positioning the pictures on the mat, Donna instantly became interested. Her eyes fell immediately on the picture of the girl walking on the motorway. Donna remarked: “That’s very dangerous”.
Further on in the course of therapy sessions, we spent time working on Donna’s exits to her unhelpful patterns of behaviour. We used ‘no entry’ signs and ‘fire exit’ signs because she knew what these meant. She told me that a ‘no entry’ meant that you could not go down that route and a ‘fire exit’ meant that you should follow that route, walking slowly and calmly.
During session 18, we positioned the pictures onto the door mat to create Donna’s reformulation diagram. Then we added all of the three exits. At this point Donna looked at the picture of the girl walking on the motorway and ripped it off, saying that she didn’t need that on there anymore. It seemed we had found a way of communicating that Donna could not only understand and actively engage with, but also a way that empowered her, giving her some control over our sessions.
During the later therapy sessions we made diagrams for each other of everything we had learnt and everything we would take away from our sessions together; I hoped this would validate our relationship. I read out my goodbye letter to Donna during the penultimate session; she told me it was really nice. The following week, for our final session, I returned with a recording of the goodbye letter on a CD for Donna. I told her that, this would mean she could listen to the letter whenever she wanted, without needing to be dependent on staff to read it out to her. On my leaving, she gave me a big hug.
Julie
Julie found it difficult when we were relying solely on verbal communication as a means of communicating in our sessions. She often found it hard to grasp some concepts I was presenting to her and the issues I was naming. In addition, I realised that Julie found it difficult at times to express herself verbally. In our early sessions, I found it problematical to get Julie to engage well in the therapy. She would often bring issues to the therapy that I thought were not obviously related to her psychological distress. It was not until I suggested that we create a tree of the people in her life that she engaged well; this was a turning point in the therapy. Julie found it easier to express herself and tell her story using different communication methods.
After this session, I revised my method of working with Julie and tried not just to rely on verbal communication. From here on we used diagrams, talking mats, drawings, feelings boards and story characters to represent emotions. My growing understanding of Julie and her individual way of communicating her internal world helped me to hypothesise and find exits towards the end of the course of therapy. One of Julie’s main exits was using an “I’m feeling” board (Diagram 5).
Diagram 5: “I’m feeling board”
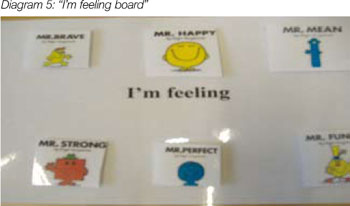
Instead of becoming upset from something and refusing help from others, after finding it hard to communicate how she was feeling, she decided to use the board to express her feelings to others around her. This enabled her to develop more helpful ways of being heard, rather than chewing her fingers and ‘throwing wobblies’ to communicate her distress about a situation. This was an example of how CAT utilises ‘scaffolding’ (Bruner, 1990), whereby the therapist supports the client to develop tools in therapy and collaboratively explores ways in which the client can use these outside of the therapy.
By using the creative approach of CAT, I feel that Julie could effectively engage with the therapy. Furthermore, I think that by using these alternative creative methods I was able to give her the opportunity to externalise the issues and alleviate some of the distress bottled up inside. Once the pattern of behaviour was mapped out onto a piece of paper and presented, we were able to see more clearly what was going on.
Concluding Thoughts
The case studies discussed illustrate how the CAT model can act as a vehicle for exploring ways of increasing psychotherapy for people with a learning disability. Both cases adopted the core features of the CAT model, such as identifying and naming reciprocal roles, looking at unhelpful patterns, presenting the client with a reformulation and finding ‘exits’.
Considerations to be taken into account when using the CAT approach within a CLDT context have been highlighted as: trust, building a therapeutic relationship, a lack of independence for clients with a learning disability, negotiating confidentiality with care staff and the cognitive ability of clients with a learning disability. Indeed, these considerations reflect the differences encountered when working with people with learning disabilities. We can see from the discussion of the therapy process that the model and therapy style was adapted to work with the personal communication style and the clients’ level of understanding.
Through looking at the two case studies presented, whilst it seems adaptations as well as a flexible approach were necessary in order for Donna and Julie to access CAT, the presence of a learning disability does not prevent an individual from actively engaging in CAT. Both Donna and Julie expressed how effective they found the sessions for making positive changes in their lives. Indeed these opinions may attract scrutiny for issues of subjectivity. However, the use of CAT with people with a learning disability is still in its infancy and to examine the effectiveness we would need to look next at what standards and outcome measures could be applied to a larger sample.
Acknowledgements
We would like to thank Hilary Brown for supervising our client work and for her support with this article.
References
Bancroft, A., Collins, S., Crowley, V., Harding, C., Kim, Y., Lloyd, J. & Murphy, N. (2008) Is CAT an island or solar system? The dilemmas in the therapeutic frame when working with people in learning disabilities services, ACAT Reformulation, Summer 2008, 23-25.
Bender, M. (1993) The unoffered chair: The history of therapeutic disdain towards people with learning difficulties, Clinical psychology forum, 54, 7-12.
Brown, M. & Marshall, K. (2006) Cognitive behavioural therapy and people with learning disabilities: Implications for developing nursing practice, Journal of psychiatric and mental health nursing, 13, 234-241.
Bruner, J. (1990) Acts of meaning, Cambridge, MA: Harvard University Press. Department of Health. (2001) Guidelines for treatment choice in psychological therapies and counselling, London: The Stationary Office.
Fisher, C. & Harding, C. (2009) Thoughts on the rebel role: Its application to challenging behaviour in learning disability services, ACAT Reformulation, Summer 2009, 4-5.
Psaila, C. L. & Crowley, V. (2006) Cognitive analytic therapy in people with learning disabilities: An investigation into the common reciprocal roles found within this client group, ACAT Reformulation, Winter 2006, 5-11.
Ryle, A. & Kerr, I. B. (2002) Introducing cognitive analytic therapy: Principles and practice, Chichester: John Wiley & Sons Ltd.
Sinason, V. (1992) Mental handicap and the mental condition: New approaches from the Tavistock, London: Free Associations.

Full Reference
Smith, H., Wills, S., 2010. Creatively Adapting CAT: Two Case Studies from a Community Learning Disability Team. Reformulation, Winter, pp.35-40.Search the Bibliography
Type in your search terms. If you want to search for results that match ALL of your keywords you can list them with commas between them; e.g., "borderline,adolescent", which will bring back results that have BOTH keywords mentioned in the title or author data.
Related Articles
Trauma, Trauma and More Trauma: CAT and Trauma in Learning Disability
Julie Lloyd, 2019. Trauma, Trauma and More Trauma: CAT and Trauma in Learning Disability. Reformulation, Summer, pp.44-46.
Val Crowley Three reflections from the CAT learning disability special interest group Phil Clayton, Julie Lloyd, Nicola Murphy
Phil Clayton, Julie Lloyd, Nicola Murphy, 2020. Val Crowley Three reflections from the CAT learning disability special interest group Phil Clayton, Julie Lloyd, Nicola Murphy. Reformulation, Summer, pp.51-52.
Cognitive Analytic Therapy & Dysphagia: using CAT relational mapping when teams can’t swallow our recommendations
Colomb, E. and Lloyd, J., 2012. Cognitive Analytic Therapy & Dysphagia: using CAT relational mapping when teams can’t swallow our recommendations. Reformulation, Winter, pp.24-27.
Thoughts on the Rebel Role: Its Application to Challenging Behaviour in Learning Disability Services
Fisher, C., Harding, C., 2009. Thoughts on the Rebel Role: Its Application to Challenging Behaviour in Learning Disability Services. Reformulation, Summer, pp.4-5.
Case Study on Z not as Impossible as we had Thought
Lloyd, J., 2007. Case Study on Z not as Impossible as we had Thought. Reformulation, Summer, pp.31-39.
Other Articles in the Same Issue
A Little Bit Of Bakhtin - From Inside To Outside And Back Again
Hepple, J., 2010. A Little Bit Of Bakhtin - From Inside To Outside And Back Again. Reformulation, Winter, pp.17-18.
A Suggested New Diagrammatic Formulation for Narcissists
Nehmad, A., 2010. A Suggested New Diagrammatic Formulation for Narcissists. Reformulation, Winter, p.44.
Accessible Snags
Melton, J., 2010. Accessible Snags. Reformulation, Winter, p.40.
Aim and Scope of Reformulation
Hepple, J., Lloyd, J., 2010. Aim and Scope of Reformulation. Reformulation, Winter, p.45.
‘When I’m The Dark Angel I Feel Worthless And Don’t Deserve Love’
Kirkland, J, 2010. ‘When I’m The Dark Angel I Feel Worthless And Don’t Deserve Love’. Reformulation, Winter, pp.19-23.
Creatively Adapting CAT: Two Case Studies from a Community Learning Disability Team
Smith, H., Wills, S., 2010. Creatively Adapting CAT: Two Case Studies from a Community Learning Disability Team. Reformulation, Winter, pp.35-40.
Financial Practicalities
Harvey, L., 2010. Financial Practicalities. Reformulation, Winter, p.46.
How Can Cognitive Analytic Therapy Contribute To The Understanding And Treatment Of “Sex Addictionâ€
Watson, R., 2010. How Can Cognitive Analytic Therapy Contribute To The Understanding And Treatment Of “Sex Addictionâ€. Reformulation, Winter, pp.13-16.
International CAT
Curran, A., Potter, S., 2010. International CAT. Reformulation, Winter, p.5.
Letter from the Chair of ACAT
Westacott, M., 2010. Letter from the Chair of ACAT. Reformulation, Winter, pp.3-5.
Letter from the Editors
Hepple, J., Lloyd, J., 2010. Letter from the Editors. Reformulation, Winter, p.3.
Letter to the Editors
Pollard, R., 2010. Letter to the Editors. Reformulation, Winter, p.5.
Mirror Workshop Summary Held On The 9th July 2010
Elia, I., 2010. Mirror Workshop Summary Held On The 9th July 2010. Reformulation, Winter, p.47.
Playfulness in CAT
Coulter, N., Rushbrook, S., 2010. Playfulness in CAT. Reformulation, Winter, pp.24-27.
Situating Social Inequality And Collective Action In Cognitive Analytic Therapy
Brown, R., 2010. Situating Social Inequality And Collective Action In Cognitive Analytic Therapy. Reformulation, Winter, pp.28-34.
The “Piacentino†Context In Which We Work As Aspiring CAT Practitioners In Italy
Fiorani, C., Poggioli, M., Provenzano, A., Romanelli, S., Sogni, A., 2010. The “Piacentino†Context In Which We Work As Aspiring CAT Practitioners In Italy. Reformulation, Winter, pp.6-11.
The Reformulation ‘16 Plus One’ Interview
Hepple, J., Lloyd, J., 2010. The Reformulation ‘16 Plus One’ Interview. Reformulation, Winter, pp.46-47.
The West Midlands CAT Practitioners Course 2009-2011
Darongkamas, J., Griffiths, Dr T., Williams, O., 2010. The West Midlands CAT Practitioners Course 2009-2011. Reformulation, Winter, pp.41-44.
Help
This site has recently been updated to be Mobile Friendly. We are working through the pages to check everything is working properly. If you spot a problem please email support@acat.me.uk and we'll look into it. Thank you.
